|
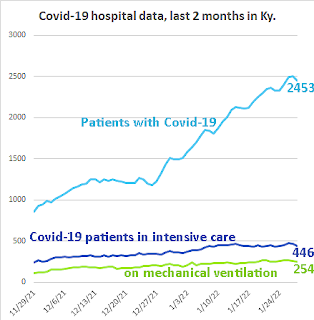
| State Dept. for Public Health graph, adapted by Ky. Health News; for a larger version, click on it. |
By Melissa Patrick
Kentucky Health News
Kentucky got a hopeful Covid-19 report from Gov. Andy Beshear at his weekly pandemic press conference, with the state's weekly coronavirus case numbers and positive-test rate on the decline.
"We certainly hope that between these two points of data, total cases and positivity rate, that we are headed in the right direction," he said.
Since Saturday, Kentucky reported 19,915 new coronavirus cases, bringing the seven-day rolling average to 10,946, 11 percent below Friday's. Of Monday's 4,950 new cases, nearly 25% are in people 18 and younger.
Kentucky reported 74,376 new cases in the Monday-to-Sunday reporting week ended Jan. 30, down from 81,473 the prior week, but still higher than two weeks ago, when the state reported 72,165 cases.
"We hope what we are seeing is a cresting and hopefully the beginning of the downward slope in Omicron cases," Beshear said.
That said, he cautioned that case numbers are still too high, noting that last week's case number was the second highest and more than double the peak during the Delta surge.
Other good news is that the weekly positivity rate, which is a leading indicator, has also gone down, and is lower than it was two weeks ago.
The share of Kentuckians testing positive for the virus in the last seven days is 28.49%, a rate that has slowly decreased since a high of 33.1% on Jan. 23.
The bad news is that hospitalizations are still going up on a weekly basis and are close to the high seen during the Delta surge. The hope, Beshear said, is that they will soon start coming down and the question is, "When and how much longer will our hospitals be pushed to the brink?"
Kentucky hospitals reported 2,413 Covid-19 patients Monday, with 454 in intensive care and 232 on mechanical ventilation. The total was 40 fewer than Friday, but it often drops on Monday, Beshear noted.
Nine of the state's 10 hospital regions continue to use at least 80% of their intensive-care beds, with four over 90%. Northern Kentucky is again at 100%.
Beshear reiterated that Kentuckians should get a Covid-19 vaccine and booster shots, pointing to an article in The New York Times that breaks down Centers for Disease Control and Prevention research that shows how getting vaccinated -- and boosted -- offers significant protection from dying from Covid-19. David Leonhardt wrote: "That risk is not zero, but it is not far from it."
The data shows that the average weekly chance of a boosted person dying of Covid was about one in a million during October and November, compared to about 2.4 per million of dying in a car crash or about three per million of dying from the flu or pneumonia, reports the Times.
"While the vaccine provides incredible protection, the booster shot provides even more,"Beshear said. "In fact, deaths of those that have gotten a booster is almost zero. Look, people are are dying because of the lack of a vaccine. These shots are safe and effective. If you haven't gotten it yet, get your vaccine. If you haven't gotten your booster, don't put it off for any reason. Go in and get it, your level of protection will be significantly increased."
So far, 2.85 million Kentuckians, 64% of the population, have received at least one dose of a Covid-19 vaccine; 2.5 million are fully vaccinated, or 55% of the total; and 1 million have been boosted, or 41.7% of the eligible population.
The statewide infection rate is 193.8 daily cases per 100,000 residents. Eight counties have rates above 300 cases per 100,000: Muhlenberg, 359.2; Hopkins, 345.6; McCracken, 343.5; Mercer, 327.6; Powell, 327.1, Clay, 320.9; Whitley, 314.4; and Hardin, 304. Every county remains red on the state incidence map, for having more than 25 daily cases per 100,000 residents, considered a high level of transmission.
The Times ranks Kentucky's seven-day infection rate third among the states, with a 32% rise in cases in the last 14 days. The rankings are based on data from the CDC, which uses different calculation methods than the state. The Times places seven Kentucky counties in the nation's top 22 in infection rate: Hopkins, Morgan, McCracken, Mercer, Boyd, Muhlenberg and Clay.
Under questioning, Beshear said he still has confidence in schools participating in the "test-to-stay" program, which allows exposed students to remain in school as long as they are not testing positive, as long as they are also enforcing a universal masking policy. Some states are moving away from this program, citing that case numbers are too high to make it effective.
"We think it is an important and valuable tool when it is paired with universal masking," Beshear said. "A test-to-stay program where you don't have universal masking might not help a lot because by the time you are doing those tests, somebody could have spread the virus to others . . . So we believe that these two mitigation tactics need to be done in concert."
The state reported 70 more Covid-19 deaths since Saturday, bringing the pandemic death toll in Kentucky to 12,960. Beshear said one of the fatalities was 38 years old and another was 42.