Events, trends, issues, ideas and independent journalism about health care and health in Kentucky, from the Institute for Rural Journalism at the University of Kentucky
Pages
Thursday, November 30, 2023
Health-care workers and public-school educators will serve as grand marshals of Gov. Andy Beshear's inauguration parade
Kentucky health-care workers and public-school educators will serve as grand marshals of Gov. Andy Beshear's inauguration parade, which is scheduled for 11 a.m. to 1 p.m. Tuesday, Dec. 12 in Frankfort. The parade will be livestreamed on KET.
“We are excited to continue moving forward, together for every Kentucky family,” the governor and first lady Britainy Beshear said in a news release. “Grand marshals for the inaugural parade represent the health-care workers who guided Kentuckians through the global pandemic, disasters and other events, and educators from across the commonwealth, who continue to lead Kentucky’s children into the future.”
The release said the parade will tells the story of Beshear’s first four-year term: "governing through a time of unprecedented adversity, capitalizing on game-changing economic opportunities and moving Kentuckians forward, together. The parade features individuals, communities, companies and groups who played a major role in the story of the last four years, looking back at the struggles and successes, before giving way to the young people who will bring Kentucky into the bright future ahead."
“Health-care workers deserve the appreciation of every Kentuckian,” said Dr. Valerie Briones-Pryor, chief medical officer at UofL Health-Shelbyville Hospital. “I’m grateful they are being honored in this way.” The official event schedule for the inauguration is here.
Uncle Sam wants you ... to help stop health-insurance companies from using misleading tactics to sell Medicare Advantage plans
 |
| iStock/Getty Images Plus illustration via KFF Health News |
KFF Health News
After an unprecedented crackdown on misleading advertising claims by insurers selling private Medicare Advantage and drug plans, the Biden administration hopes to unleash a special weapon to make sure companies follow the new rules: you.
Officials at the Centers for Medicare & Medicaid Services are encouraging seniors and other members of the public to become fraud detectives by reporting misleading or deceptive sales tactics to 1-800-MEDICARE, the agency’s 24-hour information hotline. Suspects include postcards designed to look like they’re from the government and TV ads with celebrities promising benefits and low fees that are available only to some people in certain counties.
The new rules, which took effect Sept. 30, close some loopholes in existing requirements by describing what insurers can say in ads and other promotional materials as well as during the enrollment process.
Insurance companies’ advertising campaigns are in high gear because Dec. 7 is the end of open-enrolment season, when seniors can buy policies that take effect Jan. 1. People with traditional government Medicare coverage can add or change a prescription drug plan or join a Medicare Advantage plan that combines drug and medical coverage. Although private Advantage plans offer extra benefits not available under the Medicare program, some services require prior authorization and beneficiaries are confined to a network of health care providers that can change anytime. Beneficiaries in traditional Medicare can see any provider.
Catching Medicare Advantage plans that step out of line isn’t the only reason to keep an eye out for marketing scams. Accurate plan information can help avoid enrollment traps in the first place.
Although insurers and advocates for older adults have generally welcomed the new truth-in-advertising rules, compliance is the big challenge. Expecting beneficiaries to monitor insurance company sales pitches is asking a lot, said Semanthie Brooks, a social worker and advocate for older adults in northeast Ohio. She’s been helping people with Medicare sort through their options for nearly two decades. “I don’t think Medicare beneficiaries should be the police,” she said.
Choosing a Medicare Advantage plan can be daunting. In Ohio, for example, there are 224 Advantage and 21 drug plans to choose from that take effect next year. Eligibility and benefits vary by county.
“CMS ought to be looking at how they can educate people, so that when they hear about benefits on television, they understand that this is a promotional advertisement and not necessarily a benefit that they can use,” Brooks said. “If you don’t realize that these ads may be fraudulent, then you won’t know to report them.”
Meena Seshamani, CMS’s Medicare director, told KFF Health News in a written statement that the agency relies on beneficiaries to help improve services: “The voices of the people we serve make our programs stronger,” she said, noting that complaints from policyholders prompted the government’s action. “That’s why, after hearing from our community, we took new critical steps to protect people with Medicare from confusing and potentially misleading marketing.”
Although about 31 million of the 65 million people with Medicare are enrolled in Advantage plans, even that may not be enough people to monitor the tsunami of advertising on TV, radio, the internet, and paper delivered to actual mailboxes. Last year more than 9,500 ads aired daily during the nine-week marketing period that started two weeks before enrollment opened, according to an analysis by KFF. More than 94% of the TV commercials were sponsored by health insurers, brokers, and marketing companies, compared with only 3% from the federal government touting the original Medicare program.
During just one hourlong Cleveland news program in December, researchers found, viewers were treated to nine Advantage ads.
This year, for the first time, CMS asked insurance and marketing companies this year to submit their Medicare Advantage TV ads to make sure they complied with the new rules. Officials reviewed 1,700 commercials from May 1 through Sept. 30 and nixed more than 300 they deemed misleading, according to news reports. An additional 192 ads out of 250 from marketing companies were also rejected. The agency would not disclose the total number of TV ads reviewed and rejected this year or whether ads from other media were scrutinized.
The new restrictions also apply to salespeople, whether their pitch is in an ad, written material, or a one-on-one conversation. Under one important new rule, the salesperson must explain how the new plan is different from a person’s current health insurance before any changes can be made.
That information could have helped an Indiana woman who lost coverage for her prescription drugs, which cost more than $2,000 a month, said Shawn Swindell, the State Health Insurance Assistance Program supervisor of volunteers for 12 counties in east-central Indiana. A plan representative enrolled the woman in a Medicare Advantage plan without telling her it didn’t include drug coverage, because the plan is geared toward veterans who can get drug coverage through the Department of Veterans Affairs instead of Medicare. The woman is not a veteran, Swindell said.
In New York, the Medicare Rights Center received a complaint from a man who had wanted to sign up just for a prepaid debit card to purchase nonprescription pharmacy items, said the group’s director of education, Emily Whicheloe. He didn’t know the salesperson would enroll him in a new Medicare Advantage plan that offered the card. Whicheloe undid the mistake by asking CMS to allow the man to return to his previous Advantage plan.
Debit cards are among a dizzying array of extra nonmedical perks offered by Medicare Advantage plans, along with transportation to medical appointments, home-delivered meals, and money for utilities, groceries, and even pet supplies. Last year, plans offered an average of 23 extra benefits, according to CMS. But some insurers have told the agency only a small percentage of patients use them, although actual usage is not reportable.
This month, CMS proposed additional Advantage rules for 2025 plans, including one that would require insurers to tell their members about available services they haven’t used yet. Reminders will “ensure the large federal investment of taxpayer dollars in these benefits is actually making its way to beneficiaries and are not primarily used as a marketing ploy,” officials said in a fact sheet.
Medicare Advantage members are usually locked into their plans for the year, with rare exceptions, including if they move out of the service area or the plan goes out of business. But two years ago, CMS added an escape hatch: People can leave a plan they joined based on misleading or inaccurate information, or if they discovered promised benefits didn’t exist or they couldn’t see their providers. This exception also applies when unscrupulous plan representatives withhold information and enroll people in an Advantage policy without their consent.
Another new rule that should prevent enrollments from going awry prohibits plans from touting benefits that are not available where the prospective member lives. Empty promises have become an increasing source of complaints from clients of Louisiana’s Senior Health Insurance Information Program, said its state director, Vicki Dufrene. “They were going to get all these bells and whistles, and when it comes down to it, they don’t get all the bells and whistles, but the salesperson went ahead and enrolled them in the plan.”
So, expect to see more disclaimers in advertisements and mailings like this unsolicited letter an Aetna Medicare Advantage plan sent to a New York City woman: “Plan features and availability may vary by service area,” reads one warning packed into a half-page of fine print. “The formulary and/or pharmacy network may change at any time,” it continues, referring to the list of covered drugs. “You will receive notice when necessary.”
The rules still let insurers to boast about their CMS one-to-five-star ratings, even though the ratings do not reflect the performance of specific plans that may be mentioned in an ad or displayed on the government’s Medicare plan finder website. “There is no way for consumers to know how accurately the star rating reflects the specific plan design, specific provider network, or any other specifics of a particular plan in their county,” said Laura Skopec, a senior researcher at the Urban Institute, who recently co-authored a study on the rating system.
And because ratings data can be more than a year old and plans change annually, ratings published this year don’t apply to 2024 plans that haven’t even begun yet — despite claims to the contrary.
How to spot misleading Medicare Advantage and drug plan sales pitches (and what to do about it)
The Centers for Medicare & Medicaid Services has new rules cracking down on misleading or inaccurate advertising and promotion of Medicare Advantage and drug plans. Watch out for pitches that:
- Suggest benefits are available to all who sign up when only some individuals qualify.
- Mention benefits that are not available in the service area where they are advertised (unless unavoidable because the media outlet covers multiple service areas).
- Use superlatives like “most” or “best” unless claims are backed up by data from the current or prior year.
- Claim unrealistic savings, such as $9,600 in drug savings, which apply only in rare circumstances.
- Market coverage without naming the plan.
- Display the official Medicare name, membership card, or logo without CMS approval.
- Contact you if you’re an Advantage or drug plan member and you told that plan not to notify you about other health insurance products.
- Pretend to be from the government-run Medicare program, which does not make unsolicited sales calls to beneficiaries.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at the Kaiser Family Foundation, an independent source of health policy research, polling and journalism. Reporter Susan Jaffe is at Jaffe.KHN@gmail.com.
Wednesday, November 29, 2023
Humana and Cigna, a larger insurance firm, are talking merger
 |
| Photo by Joe Bulewicz, Bloomberg News |
Louisville-based Humana Inc. is in merger talks with The Cigna Group that would create the nation's third-largest company selling health insurance.
The merger would "vault the combined company into the top tier of integrated health-care firms," The Wall Street Journal reports. "Cigna, which had revenue of about $181 billion last year, would be able to marry its huge pharmacy-benefit unit, which manages drug plans, and its strength in commercial insurance with Humana’s big position in the fast-growing Medicare segment, something Cigna has long sought."
The Journal reports, "Humana could also help Cigna accelerate a strategy that is core to the managed-care business, a move toward paying doctors and hospitals in ways that aren’t tied to the volume of service provided. These 'value-based care' setups are increasingly central to Medicare plans, but have advanced far more slowly in commercial insurance." Humana's Medicare revenue of about $93 billion last year made it the number-two Medicare insurer, after UnitedHealth; Cigna's Medicare Advantage "falls well short of that scale."
This year, Humana has "made moves that could clear the deck for a possible combination, announcing in February that it would divest its commercial business and focus on its core Medicare Advantage line. Humana has said its home-health unit and expanding primary-care footprint support its Medicare patients," the Journal notes. "The company is in the midst of its own succession handoff. Humana said in October that Jim Rechtin—previously chief executive of Envision Healthcare—would take over as president and chief operating officer, effective Jan. 8. Rechtin was then to take over as CEO from Bruce Broussard in the back half of 2024."
Tuesday, November 28, 2023
UK students planning medical careers start student organization to steer rural students into college and health-care opportunities
 |
| Jackson Miller, left, and Ethan Morgan started HealthCare Cats to help other students from rural areas navigate the many health-care education opportunities at the University of Kentucky. (UK photo) |
University of Kentucky
Jackson Miller and Ethan Morgan, former Marshall County High School classmates and now best friends and roommates at the University of Kentucky Lewis Honors College, first arrived in Lexington feeling a bit overwhelmed of all the opportunities available to them UK.
Coming from a rural area where most high-school graduates enter the workforce or the military rather than college, Miller and Morgan felt they did not have a clear roadmap of how to pursue their career aspirations of becoming physicians. To help other students not feel so lost in navigating all of the health care education opportunities, Miller and Morgan created a student organization during their sophomore year to help other students like them. The organization, HealthCare Cats, is now “providing an avenue into college and health care opportunities for rural students of Kentucky in order to create a better commonwealth.”
To start their program, Miller, a psychology major, and Morgan, a biology major, worked with several UK colleges focused on the health-care industry including the College of Medicine, College of Dentistry, College of Pharmacy and College of Nursing, for information about how to present themselves as the best candidate for those types of degrees. The students then developed a presentation that has been shared with rural high-school and college students to encourage them to aspire to a career in health care and show them the different options and opportunities that are offered at UK.
“We wanted to help students who felt behind, didn’t have the greatest study habits and most certainly weren’t aware of many of the opportunities in health care,” Miller said.
The organization, which already boasts over 160 students, will include guest speakers, networking opportunities and a mentoring program to connect first-year students with more experienced students.
“These opportunities for the members of the organization will allow us to not only reach the younger, rural generation, but also cultivate a community of future rural health leaders within the organization,” Morgan said.
Already, the organization has had speakers such as Dean Christian Brady from the Lewis Honors College, who spoke to the organization on discovering your “why” for health care and education, combating burnout, handling changes in the path of life, managing adversity in life, and more. The organization also held a graduate student panel with students from nursing, medicine, physical therapy, the physician assistant program, dentistry and pharmacy. The students shared application tips, pros and cons of their programs, and advice they would consider if they had to do it all over again.
This Friday, Dec. 1, HealthCare Cats, in partnership with the Appalachian Health Initiative, will welcome Dr. Michael D. Rankin to speak at 5 p.m. in the Lewis Honors College Scholars Lounge. Rankin, a graduate of UK, recently pledged $22 million to “advance the mission of the UK College of Medicine and expand the top-notch educational opportunities through the support of a new health education building and the funding of medical student scholarships,” as stated in the UKMedicine magazine.
“Dr. Rankin coming to speak with us will be great, for he will understand the backgrounds of our membership and be able to offer advice from the perspective of someone who has walked their paths,” Morgan said.
“Having worked with students Maddie Duff (president) and Ben Vickery in the past, it is clear that the missions of our organizations align in critical ways. Dr. Rankin speaks very highly of Appalachian students and often notes the need for them in Kentucky’s health care system. We are so excited to be able to bring in their diverse perspectives and work together to build a better commonwealth.”
Supplementing the event programming, HealthCare Cats initiated a mentorship program where rural first-year students are matched with an upper-class student to make the college/pre-health transition smoother. The first director of HealthCare Cats’ the program, Maya Moskal, is from Chicago and is considering a career in a rural market.
"Being from a bigger city, HealthCare Cats has broadened my knowledge on the health care disparities present in rural areas,” she said. “The program has opened many doors by encouraging me to give back to Kentucky, in addition to helping me personally succeed at UK in many ways.”
Through HealthCare Cats, Miller and Morgan hope to apply the common chemistry phrase “like dissolves like” by helping rural students achieve their medical aspirations — and then return to their hometowns.
Morgan asked, “Who better to serve rural populations in Kentucky than those who resided there for much of their lives?”
Monday, November 27, 2023
Over the holidays, encourage picky eaters to try something new
 |
| Photo illustration from PureWow.com |
UK HealthCare
During the holiday season, there are all kinds of foods on the table. But for parents and caregivers, even the most joyous of family gatherings can be stressful when you're dealing with a picky eater.
Sometimes what parents think is picky eating isn't actually picky eating. Some parents might be under the impression that their kids are picky eaters if they don't eat much, but children ages 2 to 5 have a slower rate of growth and therefore have smaller appetites.
It's normal for children to eat small amounts of food at one meal — sometimes just a few bites — and then a larger amount at a later meal or the next morning. They learn to regulate how much to eat and won't starve themselves. If they are growing well on their growth curves, don't worry about how much they are eating.
Keep mealtimes relaxed. The best way to prevent a child from becoming a picky eater is to make mealtimes enjoyable with a variety of small portions of healthy foods. Mealtimes should be relatively short, and children should not be made to "clean their plates." Some children will exert their independence by refusing to eat if you force them, punish them or bargain with them. The more you make them eat, the more they might begin to refuse.
Provide your child with a variety of healthy food choices in small, tablespoon-sized portions, then relax and focus on your own meal. The less focus you put on what your kid eats, the better they will eat. If they say they don't like what you have prepared, tell them that's OK and give them the same food options as the rest of the family, then return to your own meal. They will either eat, or catch up at the next meal.
Encourage your child to try new foods. A child might try a new food 10 to 15 times before realizing they actually like it. Don't be afraid to try new foods, but don't get frustrated if your child rejects them. The best way to get children to try new foods is to eat them yourself. Be sure to give them lots of praise and encouragement for taking even the smallest bite of a new food.
To help children eat better at mealtimes, follow some of these tips:
- Try to limit beverages prior to meals.
- Schedule snack time instead of letting them "graze" throughout the day.
- Serve as a role model, because children learn to feed themselves by experimenting with new foods.
- Sit at the table as a family to demonstrate healthy eating choices and habits.
Sunday, November 26, 2023
Kentucky Hospital Association says its annual survey shows state continues to have an 'acute shortage' of health care workers
 |
| Kentucky Hospital Association graph; to enlarge, click on ot; to download, right-click. |
By Melissa Patrick
Kentucky Health News
“While the shortage of health-care workers is nationwide, it has hit the commonwealth especially hard, and KHA is working with multiple partners to find ways to address the challenges,” KHA President and Chief Executive Officer Nancy Galvagni said in a news release.
The KHA Workforce Survey Report provides an in-depth look at the non-physician hospital workforce in Kentucky. It found that Kentucky had a 15% vacancy rate among that workforce in 2022.
 |
| Kentucky Hospital Association charts; click to enlarge |
The survey shows that the shortage of registered nurses is the most pronounced, with four AD districts having registered-nurse vacancies above 20 percent – Barren River (21.2%), Lincoln Trail (22.3%), Buffalo Trace (22.4%), and Bluegrass (23.7%). Vacancies employee vacancies above 20 percent, Kentucky River (23.7 percent).
“Our primary objectives are to expand Kentucky’s health care workforce pipeline, remove barriers to health care education, retain the current health care workforce, and redesign models of care,” Russell F. Cox, president and chief executive officer of Norton Healthcare and chair of the KHA Workforce Committee, said in the release. “Through extensive public and private sector collaboration, we are poised to help more Kentuckians attain rewarding, long-term careers in health care while improving the health of our communities.”
Saturday, November 25, 2023
Emergency-room visits for respiratory illness in Kentucky went up for the sixth week in a row, as hospitalizations saw a slight dip
Kentucky Health News
The breakdown of cases was 1,336 influenza, up from 1,209 the prior week; 669 were for RSV, up from 534; and 1,155 for Covid-19, down from 1,209.
Among children, hospitalizations for respiratory illness also increased in the week ended Nov. 12, to 115. That's up from 88 the week prior. Of those, 90 were for RSV, up from 67 the week before; 14 were for flu and 11 were for Covid-19, both about the same as the week prior.
In the week ended Nov. 12, Kentucky reported 3,053 laboratory-confirmed tests for Covid-19 and 424 laboratory-confirmed tests for the flu.
Covid-19 and the flu continue to kill. In the week ended Nov. 5, the state attributed four deaths to Covid-19 deaths and one to the flu.
Friday, November 24, 2023
Knowing when to choose hospice care is a challenge; that's highlighted by Rosalynn and Jimmy Carter's end-of-life journey
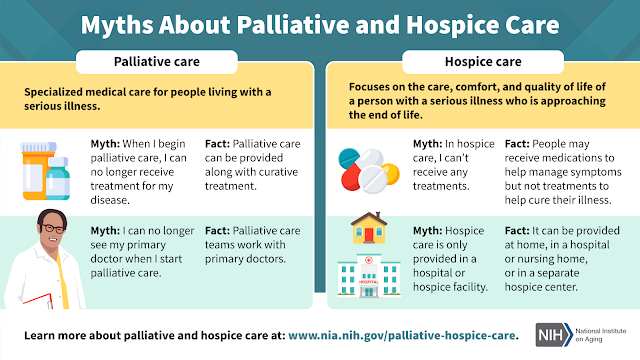 |
| National Institute on Aging infographic |
Carter, who was 96, died two days after entering hospice. Jimmy Carter entered hospice in February at the age of 98, outlasting the six-month prediction of life that is typical of people when they enter hospice care.
 |
| Rosalynn Carter (2005 Associated Press photo by Ric Feld) |
Angela Novas, senior medical officer for the Hospice Foundation of America, a nonprofit organization, told the Post that Rosalynn Carter’s experience is not uncommon.
“When people are that age and have a chronic condition like dementia that is progressing, and progressing slowly, there comes a turning point where suddenly the symptoms accelerate exponentially,” Novas said.
Doctors also play a role in delays in enrolling because of "difficulty prognosticating" and patients often wait, hoping for a final experimental treatment to become available, Mamta Bhatnagar a University of Pittsburgh Medical Center physician who specializes in hospice and palliative care, told the Post.
The first U.S. hospice opened in Connecticut 49 years ago, but there is still considerable confusion about end-of-life care options, caregivers and experts told the Post.
In contrast, “palliative care” or "comfort care" aims to make patients more comfortable and ease stress but can be done while doctors are still seeking to cure a disease.
Added to the confusion, the authors write that sometimes life-prolonging and palliative therapies can overlap, such as the use of diuretics for people with heart failure or radiation to relieve pain by shrinking a tumor.
Myths and fears about hospice still abound, Joan Teno, a Brown University hospice physician and researcher, told the Post.
“There’s very few people who say, ‘I wish I had started hospice later,’” Ben Marcantonio, interim CEO of the National Hospice and Palliative Care Organization, told the Post.
End-of-the-year holidays produce a surge in calls about hospice when families gather and physical and mental decline can become apparent, Novas told the Post. The Carters have provided a lesson in what to do next.
“The Carters are doing a fantastic job in continuing to educate us,” Novas said. “Throughout their lives, and now in their deaths, their legacy will be teaching us about mental health and how to live and how to die well.”
People seeking advice about hospice can contact the Hospice Foundation of America’s Ask an Expert service at https://hospicefoundation.org/Ask-HFA [hospicefoundation.org] or by calling 202-457-5811 or 800-854-3402.
Thursday, November 23, 2023
Bardstown woman who needs a kidney transplant testifies in Congress to change transplant policy; bill passes
 |
| LaQuayia Goldring of Bardstown prepared to testify before a U.S. Senate committee about the organ transplant process as she continues her nine year wait for a kidney. (WDRB photo) |
"I'm just asking that you all stand behind this legislation as we move forth and that all of Congress stands together to pass this legislation so more lives can be saved and less can be put in coffins," LaQuayia Goldring told senators in July.
The legislation passed, and at the end of September, President Biden signed it into law.
Goldring told Harkins that she was three years old when she was diagnosed with a rare kidney cancer. Harkins writes that Goldring "beat the cancer" in about a year, but more than a decade later she was told there were signs of kidney failure.
A week after her 17th birthday, Goldring said she learned she needed a kidney transplant and that it only took 10 days to get a match and get the procedure.
"It was able to last from the age of 17 to 25," she told Harkins. "I'm now 34. I've been waiting nine years for a kidney transplant. And our system is broken." For nine years she's been required to do dialysis treatments five days a week to stay alive.
Harkins writes that part of the waiting process is getting your name registered with the United Network for Organ Sharing, the sole organization that managed the country's organ donation policies for the past 40 years.
Just a few months ago, Harkins reports that "Goldring found out her name had been removed from the list due to a clerical error. A mistake that fueled part of her testimony in front of U.S. Senators in July."
Goldring told the senators of her struggles with UNOS and asked them to break up the UNOS monopoly and allow more contracts to be considered for handling organ transplants.
When Biden signed the legislation to do just that, Goldring told Harkins she was "overjoyed, with, with just joy and tears of relief."
"It's one thing to hear leaders, like our President, talk about organ donation and how their administration is going to do something to change it, but to actually have a law after 40 years signed doesn't get any better than that," she said.
Goldring is still waiting and praying for a life-saving donation.
"I'm just staying hopeful that that one match will come and, you know, this will be a thing of the past," she told Harkins.
According to Donate Life, more than 105,000 Americans are waiting for life-saving organ transplants, 1,000 of them Kentuckians. Goldring has a social media campaign for people who would like to see if they are eligible to donate and to follow her journey.
Wednesday, November 22, 2023
You can get four more free at-home tests for Covid-19, and if you didn't get four already, you can get eight of them, starting Monday
 |
| Photo illustration by Patrick Sison, The Associated Press |
The U.S. government is offering to send another round of four at-home virus tests ahead of the typical surge in cases during the winter holiday season.
Anyone who did not order a batch of four Covid-19 tests in September can secure up to eight of them this time around starting Nov. 27 at covidtests.gov. The U.S. Postal Service will deliver them for free.
The government is mailing out the coronavirus tests as the the flu season kicks off and a spike in respiratory syncitial virus (RSV) cases has been reported in some spots around the country. Hospitalizations for Covid-19, which has killed more than 1 million Americans, were on the rise this fall but have stayed steady in recent weeks. Immunity from previous vaccinations and infections has kept case counts lower compared with other years.
The new release of free Covid-19 nasal swab tests also comes ahead of the first winter since the pandemic started that insurers are no longer required to cover the cost of them. On average, at-home tests now cost $11 out of pocket, according to an analysis by the nonprofit Kaiser Family Foundation.
The Food and Drug Administration also approved updated Covid-19 vaccines in September in the hopes of revving up protection for Americans this winter. The shots target an omicron descendant named XBB.1.5, replacing older vaccines that targeted the original coronavirus strain and a much earlier omicron version. Shots are recommended for everyone age 6 months or older, but uptake has been slow.
U.S. taxpayers have spent tens of billions of dollars to develop Covid-19 tests, vaccines and treatments in the three years since the pandemic started.
Tuesday, November 21, 2023
Lost in the mix of 'unwinding' Medicaid to its normal procedures: The state can cut off your health care over a technical error
KFF Health News
The day her Medicaid coverage ended, Beverly Likens was in the hospital after a scary trip to the emergency room.
The resident of Martin, Ky., in Floyd County, was diagnosed with severe anemia and given a blood transfusion after her hemoglobin levels had plummeted. Likens, 48 at the time, was days from having surgery to treat chronic uterine bleeding that she said left her bleeding “constantly.”
But soon a problem appeared: The hospital said she didn’t have Medicaid coverage, jeopardizing her procedure. Likens, who is disabled, was rocked by the news. She believed she’d done what was needed to maintain her eligibility. “I was just ready to fall to pieces,” Likens said, fearing she was “going to spend the rest of my life getting blood transfusions.”
Millions of people nationwide have lost Medicaid benefits after a pandemic-era mandate for coverage expired in March — most of them for administrative reasons unrelated to their actual eligibility. Even the Biden administration and state officials had braced for complications in the historic unwinding of the continuous enrollment requirement, and had assured the public they would guard against such lapses.
Likens and an attorney who had tried to help retain her coverage said technological errors in Kentucky’s eligibility system and state missteps caused Likens’ coverage gap, throwing her surgery into limbo. As her situation demonstrates, a lapse of even a few days can have life-altering consequences.
The state never should have let Likens become uninsured, said attorney Cara Stewart, director of policy advocacy at Kentucky Voices for Health. Stewart tried to submit a new Medicaid application for Likens before her coverage stopped in June. She got stuck in a loop in Kentucky’s online system that “didn’t go away” and prevented the form from getting through. “I was just furious,” Stewart said.
Likens should never have had to reapply for coverage, Stewart said, arguing that the state violated federal regulations that say, before concluding someone is ineligible and terminating benefits, states must consider all scenarios in which someone might qualify. Likens, who doesn’t have children and isn’t working, should have qualified for Medicaid based on her income, which falls below federal limits.
Medicaid, a safety-net health program jointly run by the federal government and states, covers millions of people with disabilities, pregnant women, children, adults without children, and seniors. Often a person who qualifies for Medicaid initially for one reason could remain eligible even when life circumstances change, as long as their income remains below certain thresholds.
Before she lost her coverage, Likens qualified for Medicaid because she had Supplemental Security Income, a program for people with little to no income or assets who are blind, disabled, or at least 65 years old. Likens has multiple chronic conditions, including diabetes, hypertension, and heart disease, and said she initially got on the program after her grandfather, who supported her financially, passed away. Likens was his caretaker and didn’t go to college; following his death, she grappled with depression and anxiety that she still treats with medication and therapy.
Apart from limits on earnings, the SSI program limits beneficiaries’ assets to $2,000 for individuals and $3,000 for couples. After the Social Security Administration told her in March she was no longer eligible for SSI because she had assets whose cash value exceeded federal limits, a Kentucky agency that oversees Medicaid sent Likens a notice in April stating her health benefits would automatically stop at the end of June.
The state didn’t assess whether she qualified another way, even though regulations from the Centers for Medicare & Medicaid Services require states to consider all factors. Instead, Kentucky said she “may be eligible for Medicaid another way” and directed her to apply again.
Kentucky health officials maintained they didn’t do anything wrong. In a September letter to the Kentucky Equal Justice Center, a nonprofit that supplies legal aid, state officials said the requirement to consider whether someone qualifies for Medicaid under a different category does not apply to people with SSI benefits.
Because her Medicaid eligibility solely hinged on her receipt of SSI, “The Department for Medicaid Services does not have sufficient information on record to determine if the individual qualifies for another Medicaid type of assistance,” wrote Eric Friedlander, secretary of the Kentucky Cabinet for Health and Family Services, and Lisa Lee, commissioner of the department. “Individuals receive clear guidance in the notice they receive to file an application to determine whether they are eligible in other types of assistance.”
That explanation is “absolutely wrong,” said Elizabeth Priaulx, a senior disability legal specialist with the National Disability Rights Network. “They failed on many levels.” Priaulx pointed to policy guidance CMS issued in May, which says if a person with SSI experiences a change in circumstances, states must reassess whether they’re eligible for Medicaid in another way before terminating coverage.
Cabinet spokesman Brice Mitchell said in an email to Kentucky Health News, "This administration believes health care in a basic human right. Our work to improve health care in the commonwealth is ongoing and is something we will continue to fight for on behalf of Kentuckians. Individuals who receive Supplemental Security Income (SSI) are automatically enrolled in Medicaid . . . When an individual loses SSI benefits, several methods for retaining coverage exists. Additionally, the cabinet has health-coverage experts, known as 'kynectors,' in all 120 counties who are aware of the issue and can guide individuals to the appropriate channels for assistance."
As of 2021, there were 7.7 million SSI recipients, according to the Social Security Administration. More than 156,000 (about 148,000 disabled) were in Kentucky. The SSA has a detailed county-by county list.
Federal rules require states to first try renewing people automatically — a policy designed to help keep eligible people enrolled during what’s known as the Medicaid “unwinding.” States can do so by checking data sources, such as if a Medicaid recipient is enrolled in other public assistance programs for food and housing, or by checking federal and state income tax information. If that doesn’t work, states must send an enrollee a renewal form asking for additional information. Likens said she never got one.
All states are conducting automatic renewals for at least some enrollees. However, states generally are behind on such renewals for some beneficiaries, including seniors and people with disabilities, increasing the risk someone could lose coverage when they shouldn’t, said Joan Alker, executive director of the Georgetown University Center for Children and Families.
“Given the high level of procedural terminations, there undoubtedly are people who are eligible in another category, but they’re falling through the cracks,” Alker said.
After Likens was told to apply again for Medicaid, technological errors in Kentucky’s online system kept the application in limbo until her benefits lapsed in June, Stewart said. The state contracts with Deloitte to operate its eligibility system; a company spokesperson declined to comment.
In early July, after spending hours on the phone, Medicaid officials told her Likens’ coverage was reapproved. But it wouldn’t show up in the computer systems for Likens’ providers for days. On July 10, she received an electronic portal message from a nurse at Pikeville Medical Center saying her insurance was registering as inactive, and her surgery might be delayed as a result.
Likens replied that the state told her she was “for sure approved for coverage,” and that her updated eligibility status “should go back to active soon.” After constant calls, Stewart said, her reinstated Medicaid came through in mid-July and she had surgery July 17.
Likens was reinstated because her income was low enough. Kentucky expanded Medicaid under the Affordable Care Act, which in 2023 means a single adult without children must earn less than $20,120 annually to qualify. But she worries about others who “don’t get as lucky as I did.”
“It is not fair for any Kentuckian to have to go without health care,” she said.
Monday, November 20, 2023
UK doctor debunks myths about lung-cancer screening, which can find cancer before it spreads or causes symptoms, and save lives
 |
| Photo illustration by dragana991, iStock/Getty Images Plus |
Lung cancer is the leading cause of cancer deaths in the U.S., claiming more lives than prostate cancer, breast cancer, and colorectal cancer combined. However, it can be a curable disease if detected early through screening, which can often identify cancer before it spreads or causes symptoms.
The U.S. Preventive Services Task Force recommends annual low-dose CT scans for lung-cancer screening for individuals who meet the following criteria:
- Are 50 to 80 years old
- Currently smoke or have quit smoking within the past 15 years
- Have at least a 20 pack-year smoking history, which is determined by multiplying the number of packs a person smoked per day by the number of years the person has smoked
Myth: “Lung cancer screening is not covered by my insurance or is too expensive.”
Fact: If you meet the eligibility criteria, lung cancer screening is covered by Medicare, Medicaid and most private insurance plans without cost-sharing. In rare instances where insurance coverage is unavailable, many programs including UK’s Lung Cancer Screening Program, offer screenings at a relatively low cost.
Myth: “I quit smoking years ago, so I don't need to be screened.”
Fact: Even individuals who have quit are at high risk for lung cancer and should get screened. While screening is primarily recommended for those who quit within the past 15 years, the American Cancer Society recently expanded its guidelines to encourage screening for people with a smoking history outlined above regardless of the number of years since quitting.
Myth: “I currently smoke, so I will get screened after I quit.”
Fact: If you currently smoke, you are at the highest risk. Everyone deserves empathetic health care, and you should not feel judged or ashamed for smoking. In addition to screening, your doctor can help connect you to smoking cessation resources. Quitting smoking at any time, even after a lung cancer diagnosis, reduces the risk of dying from other diseases besides cancer, including heart and lung disease.
Myth: “Lung cancer diagnosis is a death sentence. I’d rather not know.”
Fact: A lung cancer diagnosis today is not the same as it was even 10 years ago. Surgery for lung cancer is becoming much less invasive, and improved treatment options include targeted therapy and immunotherapy. Getting screened is your best defense against lung cancer — if it’s caught early, outcomes are greatly improved, and in some cases, the cancer can be cured.
Myth: “Lung cancer screening is time-consuming and invasive.”
Fact: Lung cancer screening is less invasive than procedures like mammograms or colonoscopies. It is a painless, quick process that involves a low-dose CT scan of the chest, taking only a few minutes to complete. Minimal preparation is required, and no needles or contrast dye are used.
Myth: “Lung cancer screening has a high rate of false positives.”
Fact: While cancer screenings provide valuable tools for early detection, they also carry a potential for false positives. These results may appear as abnormalities on imaging tests but don't necessarily translate to a need for invasive procedures.
Sunday, November 19, 2023
Legislators expect to address youth vaping, maternal mortality, insurance issues and maybe abortion in upcoming session
 |
| State Rep. Kim Moser, Sen. Stephen Meredith, Rep. Rebecca Raymer and moderator Mark Marsh of Owensboro Health discuss issues at the Legislative Preview Conference. (Photo by Melissa Patrick) |
By Melissa Patrick
Kentucky Health News
State legislators expect to address youth vaping, workplace violence, data collection, maternal mortality, and prior insurance authorization for medical procedures during the legislative session that begins Jan. 2.
And they could deal with abortion. So said lawmakers who participated in a health panel or otherwise attended the Kentucky Chamber of Commerce's 2024 Legislative Preview Conference Nov. 13.
Sen. Stephen Meredith, R-Leitchfield; Rep. Kim Moser, R-Taylor Mill; and Rep. Rebecca Raymer, R-Morgantown, spent the early part of the discussion talking about health-care workforce issues and what could come out of the legislature's Certificate of Need Task Force.
Other elements of a maternal-mortality bill would involve increasing access to psychiatric care, expanding the HANDS (Health Access Nurturing Development Services) program, a voluntary home-visitation program for new or expectant parents, and also include a section about doulas, women who provide assistance during labor.
“There is some interest in our caucus in passing those exceptions,” Osborne said, adding that opinions range widely among Republicans who control the House. They also control the Senate.
Kids Count County Data Book looks at the well-being of state's children, county by county, and has some 'warning signs'
 |
| Kentucky Youth Advocates graphic |
Kentucky Health News
The 2023 Kentucky Kids Count County Data Book, which looks at the well-being of children in each county, serves as a guidepost for how Kentucky's children are doing. This year, it comes with some "warning signs."
"This year's Kids Count report, more than most, serves as a warning," Terry Brooks, executive director of Kentucky Youth Advocates, said at a Nov. 15 press conference to release the data book. "Candidly, it is not a house on fire, but it's certainly not good news."
To support his warning, Brooks noted that only 46% of the state's kindergarteners are considered ready to learn, and that worsened in 105 of the state's 169 school districts. Also, two-thirds of fourth graders do not read at the national proficiency level, and 66% of eighth graders can't meet minimal math standards.
Further, the report shows more Kentucky children are in foster care and fewer of them are being reunited with their families in 2020-22, compared to 2015-17.
Brooks called the more than 200,000 Kentucky children living poverty a "canary in the coal mine" because this number indicates where all of the other Kids Count data points are going.
"Even areas where historically we've done better, there's warning signs," he said. "For instance, we still have a very high rate of kids who are covered for health insurance. That's the good news. The bad news is, well over half the counties in Kentucky are showing a decline in that."
The percentage of Kentuckians under 19 who were covered by some form of health insurance in 2021 dropped just a bit, to 96.1%, when compared to 2016 when that rate was 96.7%. And, 97 of the state's 120 counties, or nearly 81% saw a drop in this coverage.
The County Data Book rates children's overall well being through 16 indicators in four major domains: economic security, education, family and community and health. The health indicators include smoking during pregnancy, low-birthweight babies, children under 19 with health insurance and teen births.
Statewide, the report saw improvements in the percent of Kentucky births born to women who smoke during pregnancy, to 14.2% in 2019-21, down from 18.1% in 2014-16.
Twelve Kentucky counties saw this number worsen: Ballard (17.9%), Bracken (30.1%), Calloway (14.2%), Crittenden (19.1%), Hickman (20.5%), Lawrence (27.6%), Livingston (21.3%), Lyon (21.4%), McCracken (14.4%), Trigg (19.6%), Trimble (26.6%) and Wolfe (34.8%).
Smoking during pregnancy increases the risk of health problems for developing babies, including birth before full term, low birthweight, and birth defects of the mouth and lip. Smoking during and after pregnancy also increases the risk of sudden infant-death syndrome, according to the Centers for Disease Control and Prevention.The percentage of low-birthweight babies in Kentucky stayed the same from 2014-16 to 2019-21, at 8.8%. The national average is about 8%.
A low-birthweight baby is defined as less than 5.5 pounds. The March of Dimes says babies born with low weight are more likely to have certain health conditions later in life, including diabetes, heart disease, high blood pressure, intellectual and developmental disabilities, metabolic syndrome and obesity.
Fewer teenagers are giving birth in Kentucky. The state's rate was 22.8 per 1,000 females aged 15-19 in 2019-21, down from 31.7 in 2014-16. This rate has decreased steadily since 2014-16 when that rate was 31.7 teen births per 1,000 females aged 15-19. The highest rate, 54.5, is in in Menifee County.
Twelve counties had higher teen-birth rates in 2019-21 than they did in 2014-16: Cumberland, 37.7 births per 1,000; Fleming, 34.7; Fulton, 33.7; Hickman, 37.5; Lee, 50.8; Logan, 32.4; Monroe, 41.2; Morgan, 43.1; Muhlenberg, 41.5; Owen, 27.3; Robertson, 51.1 and Washington, 24.6.
The report was made possible with support from the Casey foundation and other sponsors, including Aetna Better Health Kentucky, Kosair for Kids, Charter Communications and Mountain Comprehensive Care Center.
Saturday, November 18, 2023
Ky. kindergarteners' vaccination rates rose last year, but remained below the national average and were short of 'herd immunity' level
 |
| Graph by Kentucky Department for Public Health from state and CDC data; schools have local data. |
State law has long required the two-dose MMR vaccination for children entering school for the first time. A 2020 law allows several exemptions from vacicne mandates for "any child or adult" on religious grounds, medical reasons or a "conscientiously held belief." According to the Centers for Disease Control and Prevention, such exemptions were claimed for 1.7% of Kentucky children in 2022-23, an increase the 1.3% recorded in 2021-22.
The reported vaccination percentages may have been slightly higher because data wasn't available for about 3% of kindergarteners. At the same time, the reported figures could overstate immunity because the state counted some or all vaccine doses even if not administered at the age and time intervals the CDC recommends.
The state Department for Public Health "is working closely with local health departments across the state to promote MMR vaccination in communities that have low vaccine uptake," spokesman Brice Mitchell said in an email. "While rates have not returned to pre-pandemic levels yet, vaccination coverage in Kentucky is increasing. This highlights the need for continued education and enforcement of school and child care vaccination requirements in Kentucky to ensure the health and safety of all children. . . . Vaccination is a simple, safe and effective way to protect against harmful diseases."
 |
| Graph by Your Local Epidemiologist from CDC data, adapted by Ky. Health News; click to enlarge. |



