Events, trends, issues, ideas and independent journalism about health care and health in Kentucky, from the Institute for Rural Journalism at the University of Kentucky
Pages
▼
Sunday, December 31, 2017
Here are some expert tips for making and keeping New Year's resolutions that will stick, and help improve your health
 |
| Dreamstime.com |
Kentucky Health News
It's time again to make those New Year's resolutions. A recent national poll found that some of the most popular resolutions have to do wiht health: losing weight, exercising more, eating healthier and kicking the smoking habit.
These are all admirable goals, and some that many Kentuckians-- who lead the nation in poor health, obesity and smoking -- could take to heart, the problem seems to be sticking to them.
According to Statistic Brain, a survey-based research institute, 41 percent of Americans make a New Year's resolution, but fewer than 10 percent of them are successful, and over 40 percent of those who make a resolution will give up before the end of January, The Wall Street Journal reports.
A national poll conducted by the Marist College Institute for Public Opinion offers a bit more hope, reporting that 44 percent who make a resolution will keep it, and that 68 percent of those who made a resolution in 2017 said they kept at least a portion of the promise.
So you might ask, why even bother?
Research conducted by Dr. John Norcross, a psychology professor at the University of Scranton, found that people are 10 times more likely to make a change by declaring a New Year's resolution compared to "non-resolvers." It also found that 44 percent of people who make a resolution are successful six months into the new year, ABC News reports.
The American Psychological Association offers several, common-sense suggestions to get started.
First, the psychologists say, start small and change only one behavior at a time. For example, if your overarching goal is to eat healthier, commit to eating one serving of fresh fruits or vegetables with each meal instead of seeing your diet as a form of punishment.
They also encourage community, noting that finding a support group increases your odds of success. And don't beat yourself up, they say, missteps are normal. Finally, they suggest seeking professional help from a psychologist or other professional if you need help changing unhealthy behaviors or addressing emotional issues.
“Setting small, attainable goals throughout the year, instead of a singular, overwhelming goal on January 1 can help you reach whatever it is you strive for,” psychologist Lynn Bufka told the association. “Remember, it is not the extent of the change that matters, but rather the act of recognizing that lifestyle change is important and working toward it, one step at a time.”
The New York Times sums up these ideas nicely, saying it's time for us to "resolve to set better resolutions." This author suggests we need to make sure we are resolving to change something we want to change, and not what society is telling us to change, adding that our resolutions should be clearly defined and realistic.
ABC adds that it's important to dig deep and make sure you know why you are making the resolution. For example, we all know that we need to eat better and exercise more, but the why of doing this could be different for each of us. For example, for some it could be to reduce their cholesterol levels or to get off their Type 2 diabetes medicine, but for others it may simply be to live long enough to know their grandchildren.
A separate New York Times article recommends using the SMART method when making New Year's resolutions -- an acronym that was coined in the journal Management Review in 1981 as a guideline for making goals that are Specific, Measurable, Achievable, Relevant and Timely.
If you need help picking a resolution, Newsweek offers 15 simple resolutions that are linked to research supporting why they would be meaningful; many of them are related to improving your health. The first suggestion is to eat more fish, linking to another article full of research showing why that's a good idea. One example: Eating more fish helps children sleep better, improve their IQs and avoid heart disease. Some of the magazine's easy, health-related resolutions include preparing a meal at least once a week, eating a salad once a week, and spending more time outside.
USA Today, in an article originally published in Exact Sciences, also offers five easy resolutions to make and keep, with supporting evidence on how they will improve your health. They include flossing daily, scheduling a physical examination, eating vegetables instead of drinking them, eating more slowly and chewing your food longer, and going to bed 15 minutes earlier.
Friday, December 29, 2017
Marijuana and vaping are more popular than tobacco cigarettes among U.S. teens, but in Ky. use of the three are about equal
By Melissa Patrick
Kentucky Health News
More American teenagers are using marijuana and vaping than are smoking cigarettes, but Kentucky teens use the three products about equally, according to national and state surveys of them.
The national "Monitoring the Future" survey found that in 2017, 23.9 percent of high-school seniors reported using marijuana in the 30 days before the survey, while 9.7 percent reported smoking tobacco during that period. The survey found that 16.6 percent had used electronic cigarettes, which can be vaped with marijuana products.
Among sophomores across the nation, 15.2 percent reported using marijuana, 13.1 percent vaping and 5 percent tobacco cigarettes. Among eighth-graders, 5.5 percent reported using marijuana, 6.6 percent vaping and 1.9 percent tobacco.
The MTF survey, which has tracked substance-use trends among students for 43 years, is conducted annually by the Institute for Social Research at the University of Michigan and is funded by the National Institute on Drug Abuse. The latest survey included about 44,000 students in 360 public and private schools.
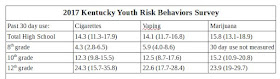
The survey doesn't produce state-by-state data, but the Kentucky Youth Risk Behavior Survey in 2017 found that Kentucky's high-school students used the three products at about the same rate.
The state survey found that 14.3 percent of Kentucky's high-school students reported smoking tobacco cigarettes, 14.1 percent vaping and 15.8 percent using marijuana in the 30 days prior to the survey. The differences in the numbers are not large enough to be statistically significant.
The Kentucky results among the three grades were also close. Among eighth graders, 5.9 percent reported vaping and 4.3 percent of them reported smoking tobacco cigarettes in the 30 days before being surveyed. On marijuana, the survey didn't specify a time period, but only asked if they had ever used marijuana; 11.9 percent said they had.
Vaping
Both surveys found the percentage of students who used electronic cigarettes remained the same since the previous poll. For the first time, the national survey asked what substances the students thought they were vaping.
It found that during the past year, about one in 10 seniors said they thought they had vaped marijuana, as had 8 percent of 10th graders and 3 percent of 8th graders.
About one in 20 of the seniors said they thought they had vaped nicotine in the past year, as had 16 percent and 8 percent of 10th and 8th graders, respectively.
During the last time they vaped, 74.8 percent of eighth graders, 59.2 percent of sophomores and 51.8 percent of seniors said they thought they had used "just flavoring." The University of Michigan news release notes that it is possible that these students are getting nicotine, but are not aware of it.
"These findings emphasize that vaping has progressed well beyond a cigarette alternative," principal researcher Richard Miech said in the release. "Vaping has become a new delivery device for a number of substances, and this number will likely increase in the years to come."
Marijuana
The release said the national survey found "the first significant increase in seven years" in marijuana use, 1.3 percent. The Kentucky rate remained stable.
The national survey found 13.5 percent of eighth graders had ever used marijuana; in Kentucky the figure was 11.9 percent. Among U.S. 10th graders, the figure was 30.7 percent; among those in Kentucky, it was 32.5 percent. Among seniors, it was 45 percent nationwide and 46.5 percent in Kentucky.
The national survey also found that the daily use of marijuana has become "as, or more, popular" among teens as daily smoking of tobacco cigarettes. Among high-school seniors, 5.9 percent said they used marijuana daily; 4.2 percent said they were daily cigarette smokers. The Kentucky survey didn't measure daily marijuana use, but found that 8.9 percent of the state's seniors are daily tobacco smokers.
The national increase in marijuana use “has been expected by many,” Miech said. “Historically, marijuana use has gone up as adolescents see less risk of harm in using it. We’ve found that the risk adolescents see in marijuana use has been steadily going down for years to the point that it is now at the lowest level we’ve seen in four decades.”
In 1991, 41 percent of seniors said they saw "great risk" in occasionally smoking marijuana; in 2017, only 14 percent said that.
The biennial Kentucky Incentives for Prevention Survey, which also asks students about substance use but also their perceptions of it, found that the perception of "great risk" for occasional marijuana use was higher in Kentucky than nationally, but is also dropping: 43.1 percent of Kentucky high-school seniors said smoking marijuana once or twice a week posed "moderate" or "great risk," down greatly from 75.5 percent in 2004.
The national survey found that high-school seniors in states allowing the medical use of marijuana are more likely to have vaped marijuana and consumed marijuana edibles than in states without such laws. For example, in states with medical-marijuana laws, 16.7 percent of seniors said they had consumed marijuana edibles, while only 8.3 percent had done so in states without such laws.
Kentucky legislators who chair the House and Senate health committees indicated on the Dec. 18 "Kentucky Tonight" on KET that medical marijuana will be discussed more than before in the upcoming legislative session. They also said more action will be taken against the opioid epidemic.
Opioids
The national survey's best news was the low levels of opioid use by youth, noting that the misuse of prescription drugs like Vicodin and OxyContin and heroin are at record low levels among both middle- and high- school students.
The national survey found that 4.2 percent of high-school seniors in this year's survey reported misusing "narcotics other than heroin" in the past year, compared to 9.5 percent in 2004, the peak year of opioid misuse in the survey. The survey only asks this question of seniors.
In 2017, 12.6 percent of Kentucky seniors said they had taken "pain medicine without a doctor's prescription or differently than how a doctor told them to use it," compared to 2011 (the first year the state survey asked this question), when the rate was 20.9 percent.
This rate also dropped for Kentucky's 10th graders, to 10.8 percent in 2017 from 16.3 percent in 2011. Among eighth graders, it has ranged from as low as 5.3 percent in 2017 to as high as 11.2 percent in 2013.
The Michigan researchers say they hope that the low opioid-misuse rates will follow U.S. teens into adulthood, since it is well established that the risk of addiction increases when drug use begins during adolescence or earlier.
Alcohol
Nationally and in Kentucky, alcohol use has been trending down, but the declines have slowed.
For example, this year's national measure of binge drinking (five or more drinks on a single occasion in the past 30 days) results didn't show much difference from last year, with 16.6 percent of high-school seniors reporting binge drinking in the previous two weeks; 9.8 percent of 10th graders and 3.7 percent of 8th graders.
The state survey found 23.8 percent of seniors and 11.2 percent of sophomores reported binge drinking. The survey did not ask eighth graders this question.
Kentucky Health News
More American teenagers are using marijuana and vaping than are smoking cigarettes, but Kentucky teens use the three products about equally, according to national and state surveys of them.
The national "Monitoring the Future" survey found that in 2017, 23.9 percent of high-school seniors reported using marijuana in the 30 days before the survey, while 9.7 percent reported smoking tobacco during that period. The survey found that 16.6 percent had used electronic cigarettes, which can be vaped with marijuana products.
Among sophomores across the nation, 15.2 percent reported using marijuana, 13.1 percent vaping and 5 percent tobacco cigarettes. Among eighth-graders, 5.5 percent reported using marijuana, 6.6 percent vaping and 1.9 percent tobacco.
The MTF survey, which has tracked substance-use trends among students for 43 years, is conducted annually by the Institute for Social Research at the University of Michigan and is funded by the National Institute on Drug Abuse. The latest survey included about 44,000 students in 360 public and private schools.
 |
| Figures in parentheses give the possible range of results within margin of error. |
The state survey found that 14.3 percent of Kentucky's high-school students reported smoking tobacco cigarettes, 14.1 percent vaping and 15.8 percent using marijuana in the 30 days prior to the survey. The differences in the numbers are not large enough to be statistically significant.
The Kentucky results among the three grades were also close. Among eighth graders, 5.9 percent reported vaping and 4.3 percent of them reported smoking tobacco cigarettes in the 30 days before being surveyed. On marijuana, the survey didn't specify a time period, but only asked if they had ever used marijuana; 11.9 percent said they had.
Vaping
Both surveys found the percentage of students who used electronic cigarettes remained the same since the previous poll. For the first time, the national survey asked what substances the students thought they were vaping.
 |
| NIH graphic |
About one in 20 of the seniors said they thought they had vaped nicotine in the past year, as had 16 percent and 8 percent of 10th and 8th graders, respectively.
During the last time they vaped, 74.8 percent of eighth graders, 59.2 percent of sophomores and 51.8 percent of seniors said they thought they had used "just flavoring." The University of Michigan news release notes that it is possible that these students are getting nicotine, but are not aware of it.
"These findings emphasize that vaping has progressed well beyond a cigarette alternative," principal researcher Richard Miech said in the release. "Vaping has become a new delivery device for a number of substances, and this number will likely increase in the years to come."
Marijuana
The release said the national survey found "the first significant increase in seven years" in marijuana use, 1.3 percent. The Kentucky rate remained stable.
The national survey found 13.5 percent of eighth graders had ever used marijuana; in Kentucky the figure was 11.9 percent. Among U.S. 10th graders, the figure was 30.7 percent; among those in Kentucky, it was 32.5 percent. Among seniors, it was 45 percent nationwide and 46.5 percent in Kentucky.
The national survey also found that the daily use of marijuana has become "as, or more, popular" among teens as daily smoking of tobacco cigarettes. Among high-school seniors, 5.9 percent said they used marijuana daily; 4.2 percent said they were daily cigarette smokers. The Kentucky survey didn't measure daily marijuana use, but found that 8.9 percent of the state's seniors are daily tobacco smokers.
The national increase in marijuana use “has been expected by many,” Miech said. “Historically, marijuana use has gone up as adolescents see less risk of harm in using it. We’ve found that the risk adolescents see in marijuana use has been steadily going down for years to the point that it is now at the lowest level we’ve seen in four decades.”
In 1991, 41 percent of seniors said they saw "great risk" in occasionally smoking marijuana; in 2017, only 14 percent said that.
The biennial Kentucky Incentives for Prevention Survey, which also asks students about substance use but also their perceptions of it, found that the perception of "great risk" for occasional marijuana use was higher in Kentucky than nationally, but is also dropping: 43.1 percent of Kentucky high-school seniors said smoking marijuana once or twice a week posed "moderate" or "great risk," down greatly from 75.5 percent in 2004.
The national survey found that high-school seniors in states allowing the medical use of marijuana are more likely to have vaped marijuana and consumed marijuana edibles than in states without such laws. For example, in states with medical-marijuana laws, 16.7 percent of seniors said they had consumed marijuana edibles, while only 8.3 percent had done so in states without such laws.
Kentucky legislators who chair the House and Senate health committees indicated on the Dec. 18 "Kentucky Tonight" on KET that medical marijuana will be discussed more than before in the upcoming legislative session. They also said more action will be taken against the opioid epidemic.
Opioids
The national survey's best news was the low levels of opioid use by youth, noting that the misuse of prescription drugs like Vicodin and OxyContin and heroin are at record low levels among both middle- and high- school students.
The national survey found that 4.2 percent of high-school seniors in this year's survey reported misusing "narcotics other than heroin" in the past year, compared to 9.5 percent in 2004, the peak year of opioid misuse in the survey. The survey only asks this question of seniors.
The percentages of high-school and middle-school students misusing prescription drugs has also dropped in Kentucky, but remain higher than the national rates.
In 2017, 12.6 percent of Kentucky seniors said they had taken "pain medicine without a doctor's prescription or differently than how a doctor told them to use it," compared to 2011 (the first year the state survey asked this question), when the rate was 20.9 percent.
This rate also dropped for Kentucky's 10th graders, to 10.8 percent in 2017 from 16.3 percent in 2011. Among eighth graders, it has ranged from as low as 5.3 percent in 2017 to as high as 11.2 percent in 2013.
Alcohol
Nationally and in Kentucky, alcohol use has been trending down, but the declines have slowed.
For example, this year's national measure of binge drinking (five or more drinks on a single occasion in the past 30 days) results didn't show much difference from last year, with 16.6 percent of high-school seniors reporting binge drinking in the previous two weeks; 9.8 percent of 10th graders and 3.7 percent of 8th graders.
The state survey found 23.8 percent of seniors and 11.2 percent of sophomores reported binge drinking. The survey did not ask eighth graders this question.
Flu blamed for deaths of three elderly people in Lexington
 |
| Herald-Leader photo by Charles Bertram |
Lexington-Fayette County Health Department spokesman Kevin Hall told WKYT-TV that the three had other health complications, but flu was the proximate cause of their deaths.
Flu cases had been confirmed in 14 of Kentucky's 17 health regions as of Dec. 16, the last weekly flu report from the state Department for Public Health. The peak of the flu season, late January and early February, is approaching, but it usually runs into May, so health officials recommend that everyone get a flu shot. Many pharmacies across the state still offer the shots.
Wednesday, December 27, 2017
The chronic pain of fibromyalgia, often worse in the winter, can still be effectively managed and treated, doctor writes
Winter can be tough for people with fibromyalgia, "a complex, long-term illness that causes severe musculoskeletal pain and fatigue," and affects women more than men, Dr. Indhira Bisono-Jimenez of KentuckyOne Health Rheumatology Associates writes for the Lexington Herald-Leader.
"Chronic feelings of intense joint or muscle pain and increased fatigue are the most prominent symptoms of
fibromyalgia," Bisono-Jimenez writes. "Other symptoms might include depression, anxiety, stress,
sleep deprivation, headaches or migraines, tingling or numbness in the
hands and feet, and problems with the digestive system, such as
constipation and irritable bowel syndrome."
Fortunately, the doctor writes, fibromyalgia can be "effectively treated and managed," with "narcotic medications used to relieve intense pain, duloxetine or milnacipran to treat pain and fatigue, pregabalin for nerve pain, and over-the-counter medications such as ibuprofen, aspirin or naproxen.
A series of therapeutic treatment options are often recommended to alleviate pain. Massage therapy, chiropractic therapy, movement therapy and acupuncture are all recommended as a supplement to reducing pain and treating fibromyalgia. Physical and occupational therapy are often recommended as well, along with counseling to help sufferers learn strategies to better manage stress."
Aside from medicine and therapy, doctors may also recommend lifestyle changes to help treat and manage fibromyalgia. Those include "getting plenty of sleep and exercising regularly," Bisono-Jimenez writes. "Walking, biking or swimming at least 30 minutes a day, five days a week is often recommended. Maintaining a proper diet, getting enough sleep and modifying workloads are also key to effectively managing fibromyalgia."
 |
| Dr. Indhira Bisono-Jimenez |
Fortunately, the doctor writes, fibromyalgia can be "effectively treated and managed," with "narcotic medications used to relieve intense pain, duloxetine or milnacipran to treat pain and fatigue, pregabalin for nerve pain, and over-the-counter medications such as ibuprofen, aspirin or naproxen.
A series of therapeutic treatment options are often recommended to alleviate pain. Massage therapy, chiropractic therapy, movement therapy and acupuncture are all recommended as a supplement to reducing pain and treating fibromyalgia. Physical and occupational therapy are often recommended as well, along with counseling to help sufferers learn strategies to better manage stress."
Aside from medicine and therapy, doctors may also recommend lifestyle changes to help treat and manage fibromyalgia. Those include "getting plenty of sleep and exercising regularly," Bisono-Jimenez writes. "Walking, biking or swimming at least 30 minutes a day, five days a week is often recommended. Maintaining a proper diet, getting enough sleep and modifying workloads are also key to effectively managing fibromyalgia."
Saturday, December 23, 2017
Tips for healthy holiday cooking and eating out
Eating healthy and sticking to a diet can be tough during the holidays. Here are some tips to help you enjoy holiday festivities while maintaining a healthy, well balanced diet, from the Kentucky Department for Public Health (if you're reading this after the holidays, save it for next year):
- During meal planning and preparation, choose recipes that can be easily made in bulk. Leftovers from these dishes can be good options for weekday lunches or dinners, and offer some extra savings.
- When prepping your meals choose one or two simple recipes. Two examples are sheet pan fajitas or Greek chicken bowls.
- When grocery shopping, buy enough recipe ingredients (i.e. lean protein, whole grains, and vegetables) for five meals.
- Cook all the food at once (for example, a large batch of brown rice, a sheet pan full of chicken and vegetables); and portion the food into reusable containers and store in the refrigerator until needed.
Holiday events make grabbing a quick bite on the go or going out to dinner more likely at this time. The health department has tips for eating out during the holidays:
- Share an entrée with someone else. The portions are often large enough to easily split a meal.
- Choose an entrée with lots of vegetables, since they contain fiber and other nutrients to help you stay full longer without going overboard on calories. The more vegetables, the better!
- Ask the server to bring out a to-go box as soon as your meal comes. Pack half of it up before starting to eat. Save the rest for lunch the next day.
- Don't be afraid to ask what is in your food and request changes. Order the way you want it.
More tips on cooking can be seen in Cooking Healthy with Secretary Glisson, a video with Health Secretary Vickie Yates Brown Glisson.
Friday, December 22, 2017
Poor adults on Medicaid more likely to quit smoking in expansion states like Ky.; 26 % of Ky. smokers use cessation benefit
Corrective Notice: If your publication has used this story, please use this revised story or post a correction on the original to reflect that 26 percent of Kentucky's Medicaid smokers used the smoking cessation benefit during the 2016-17 fiscal year, and not 15 percent as originally reported. The original calculation did not take into account that of the 1.4 million Kentuckians on Medicaid, only about 800,000 of them are adults. Please note that the headline has also been corrected.
By Melissa Patrick
Kentucky Health News
Low-income adults who gained health insurance under the expansion of Medicaid like Kentucky and most other states were more likely to quit smoking than those in states that didn't expand the program.
So says a study by the University of Pittsburgh Graduate School of Public Health, published in the journal Medical Care. Researchers examined smoking-related responses from more than 36,000 low-income adults without dependent children using data from the federal Centers for Disease Control and Prevention's Behavioral Risk Factor Surveillance Survey for the years 2011 to 2015.
It found that in the 31 states that expanded Medicaid, 8.1 percent of those newly covered said they had quit smoking in the past year, compared with 6 percent of low-income adults in states that did not expand Medicaid. (This was after the researchers factored in the effects of smoking rates from demographics, differences in cigarette taxes and states' indoor-air smoking policies.)
“Smoking cessation is notoriously difficult to achieve,” Marian Jarlenski, senior author and assistant professor in Pitt's Department of Health Policy and Management, said in a news release. “The sizable increase we found in smoking cessation might lead to significant reductions in death and diseases caused by smoking, and the taxpayer-funded health care expenditures that come with treating them.”
The report notes that smoking is responsible for 9 percent of annual health-care spending in the U.S. The annual cost of smoking related health care costs to Kentucky is estimated to be $1.92 billion.
J. Wyatt Koma, a lead author of the study, said there are many ways that engaging with health-care services could motivate new Medicaid enrollees to stop smoking.
“During the Medicaid enrollment process, people are asked whether they smoke, so it’s possible that this question might prompt them to start contemplating smoking cessation," he said in the release. "After enrollment, they have access to primary-care visits, where their clinician is likely to counsel them about quitting. And studies have shown that people in states with Medicaid expansion are much more likely to get prescriptions for smoking-cessation medications, which are covered by Medicaid.”
The researchers say the study provides evidence that Medicaid coverage can help people stop smoking. Koma said the quit rate of 8.1 percent is low, especially compared to the almost 70 percent of adults who say they want to quit.
What about Kentucky?
About 30 percent of low-income adults in the United States are smokers, which is double the national average. That rate is even higher among Kentucky's Medicaid population -- almost 44 percent, according to a survey conducted by the federal Center for Medicare and Medicaid Services.
That means 616,000 of the approximately 1.4 million Kentuckians on Medicaid are smokers. In the 2016-17 fiscal year, 90,013 of them used the smoking-cessation benefit -- about 15 percent of the smokers.
Of those, 49,319 were on Medicaid due to the expansion, which covers about 480,000 people, and 40,694 were on traditional Medicaid, according to the state Department of Medicaid Services. The expansion took effect in 2014.
The figures shows only how many Medicaid beneficiaries used the smoking-cessation benefit and not how many of them were successful at quitting.
A similar look at Medicaid claims data from 2015 found that only 17.2 percent of Medicaid smokers used a smoking-cessation medication and a mere 1.4 percent received smoking-cessation counseling. The 2015 Cabinet for Health and Family Services report cited a much smaller number of Kentuckians on Medicaid dependent on tobacco, only 10 percent, but that data was based partly on records that were likely incomplete.
New law and advocacy could lead to higher participation
When the numbers for the current fiscal year are compiled, they could show increased use of the smoking-cessation benefit, because Kentucky passed a law in the 2017 legislative session to require all health insurers, including Medicaid managed-care companies, to remove barriers to coverage for all federally approved tobacco-cessation medications and programs. The law took effect June 29, the day before the fiscal year ended.
Why was the law needed, if the Patient Protection and Affordable Care Act requires all insurance policies to cover smoking-cessation treatments? Insurers erected several barriers to treatment, such as co-payments, prior-authorization requirements and limits on length of treatment.
One of the goals of the newly formed Coalition for a Smoke-Free Tomorrow, staffed by the Foundation for a Healthy Kentucky, is to educate the public and health-care providers about the new law.
“We are all working to educate physicians, community health workers and residents to ensure they know that counseling and nicotine-replacement therapies are available free of charge," said Ben Chandler, president and CEO of the foundation. "The starting points for smokers vary; it may be a talk with their doctor, or seeing one of the ads for the Kentucky QuitLine campaign. Our goal is to make sure that every Kentuckian who is addicted to nicotine knows where they can get the help they need to successfully kick the habit.”
Resources to help Kentuckians quit smoking can be found at www.quitnowkentucky.org and www.smokefreetomorrow.org. Kentucky's Tobacco Quitline is 1-800-QUIT-NOW (1-800-784-8669). Also, many local health departments offer smoking cessation classes.
By Melissa Patrick
Kentucky Health News
Low-income adults who gained health insurance under the expansion of Medicaid like Kentucky and most other states were more likely to quit smoking than those in states that didn't expand the program.
So says a study by the University of Pittsburgh Graduate School of Public Health, published in the journal Medical Care. Researchers examined smoking-related responses from more than 36,000 low-income adults without dependent children using data from the federal Centers for Disease Control and Prevention's Behavioral Risk Factor Surveillance Survey for the years 2011 to 2015.
It found that in the 31 states that expanded Medicaid, 8.1 percent of those newly covered said they had quit smoking in the past year, compared with 6 percent of low-income adults in states that did not expand Medicaid. (This was after the researchers factored in the effects of smoking rates from demographics, differences in cigarette taxes and states' indoor-air smoking policies.)
“Smoking cessation is notoriously difficult to achieve,” Marian Jarlenski, senior author and assistant professor in Pitt's Department of Health Policy and Management, said in a news release. “The sizable increase we found in smoking cessation might lead to significant reductions in death and diseases caused by smoking, and the taxpayer-funded health care expenditures that come with treating them.”
The report notes that smoking is responsible for 9 percent of annual health-care spending in the U.S. The annual cost of smoking related health care costs to Kentucky is estimated to be $1.92 billion.
J. Wyatt Koma, a lead author of the study, said there are many ways that engaging with health-care services could motivate new Medicaid enrollees to stop smoking.
“During the Medicaid enrollment process, people are asked whether they smoke, so it’s possible that this question might prompt them to start contemplating smoking cessation," he said in the release. "After enrollment, they have access to primary-care visits, where their clinician is likely to counsel them about quitting. And studies have shown that people in states with Medicaid expansion are much more likely to get prescriptions for smoking-cessation medications, which are covered by Medicaid.”
About 30 percent of low-income adults in the United States are smokers, which is double the national average. That rate is even higher among Kentucky's Medicaid population -- almost 44 percent, according to a survey conducted by the federal Center for Medicare and Medicaid Services.
Of those, 49,319 were on Medicaid due to the expansion, which covers about 480,000 people, and 40,694 were on traditional Medicaid, according to the state Department of Medicaid Services. The expansion took effect in 2014.
The figures shows only how many Medicaid beneficiaries used the smoking-cessation benefit and not how many of them were successful at quitting.
A similar look at Medicaid claims data from 2015 found that only 17.2 percent of Medicaid smokers used a smoking-cessation medication and a mere 1.4 percent received smoking-cessation counseling. The 2015 Cabinet for Health and Family Services report cited a much smaller number of Kentuckians on Medicaid dependent on tobacco, only 10 percent, but that data was based partly on records that were likely incomplete.
New law and advocacy could lead to higher participation
When the numbers for the current fiscal year are compiled, they could show increased use of the smoking-cessation benefit, because Kentucky passed a law in the 2017 legislative session to require all health insurers, including Medicaid managed-care companies, to remove barriers to coverage for all federally approved tobacco-cessation medications and programs. The law took effect June 29, the day before the fiscal year ended.
Why was the law needed, if the Patient Protection and Affordable Care Act requires all insurance policies to cover smoking-cessation treatments? Insurers erected several barriers to treatment, such as co-payments, prior-authorization requirements and limits on length of treatment.
One of the goals of the newly formed Coalition for a Smoke-Free Tomorrow, staffed by the Foundation for a Healthy Kentucky, is to educate the public and health-care providers about the new law.
“We are all working to educate physicians, community health workers and residents to ensure they know that counseling and nicotine-replacement therapies are available free of charge," said Ben Chandler, president and CEO of the foundation. "The starting points for smokers vary; it may be a talk with their doctor, or seeing one of the ads for the Kentucky QuitLine campaign. Our goal is to make sure that every Kentuckian who is addicted to nicotine knows where they can get the help they need to successfully kick the habit.”
Resources to help Kentuckians quit smoking can be found at www.quitnowkentucky.org and www.smokefreetomorrow.org. Kentucky's Tobacco Quitline is 1-800-QUIT-NOW (1-800-784-8669). Also, many local health departments offer smoking cessation classes.
Flu is 'widespread' in Ky., with one flu-related adult death reported; still time to get a flu shot, as season goes through May
Kentucky's influenza level has just been upgraded to "widespread," prompting state health officials to redouble their advice to Kentuckians to get a flu shot and keep their hands washed.
“With current widespread flu activity being reported in Kentucky, it is a still a good time to protect yourself and your family by getting a flu shot," Dr. Jeffrey Howard, the state's acting health commissioner, said in a news release. “The Department for Public Health is strongly urging anyone who hasn’t received a flu vaccine, particularly children 6 months and older and those people at high risk for complications related to the flu, to check with local health departments or other providers about getting the vaccine.”
A "widespread" classification, the highest level of flu activity, is used when at least half of the state's 17 health regions have increased flu activity.
As of Dec. 16, Kentucky had 350 laboratory-confirmed cases of flu, with just over half between Dec. 10 and 16, according to the weekly influenza surveillance report.
The report says there has been one flu-related adult death this season and seven outbreaks in the state's nursing homes.
Flu is very contagious and is especially dangerous to small children, the elderly and those who have chronic health conditions. It is caused by a virus that spreads from person to person. Symptoms include fever, headache, cough, sore throat, runny nose, sneezing and body aches.
Persons who develop symptoms should contact their medical provider to determine if they are a good candidate for treatment with an antiviral drug, which could shorten the course of the illness or reduce its severity.
The Centers for Disease Control and Prevention recommends that everyone over six months of age get a flu vaccination, and especially encourages people who may be at higher risk for complications or negative consequences get one. It takes about 2 weeks following the administration of the vaccine for the recipient to develop protection from the flu.
The CDC offers these tips to stop the spread of germs:
“With current widespread flu activity being reported in Kentucky, it is a still a good time to protect yourself and your family by getting a flu shot," Dr. Jeffrey Howard, the state's acting health commissioner, said in a news release. “The Department for Public Health is strongly urging anyone who hasn’t received a flu vaccine, particularly children 6 months and older and those people at high risk for complications related to the flu, to check with local health departments or other providers about getting the vaccine.”
As of Dec. 16, Kentucky had 350 laboratory-confirmed cases of flu, with just over half between Dec. 10 and 16, according to the weekly influenza surveillance report.
The report says there has been one flu-related adult death this season and seven outbreaks in the state's nursing homes.
Flu is very contagious and is especially dangerous to small children, the elderly and those who have chronic health conditions. It is caused by a virus that spreads from person to person. Symptoms include fever, headache, cough, sore throat, runny nose, sneezing and body aches.
Persons who develop symptoms should contact their medical provider to determine if they are a good candidate for treatment with an antiviral drug, which could shorten the course of the illness or reduce its severity.
The CDC offers these tips to stop the spread of germs:
- Avoid close contact with sick people.
- While sick, limit contact with others.
- If you have the flu, stay home for at least 24 hours after your fever is gone (without the use of fever-reducing medicines) except to get medical care or for other necessities.
- Cover your nose and mouth with a tissue when you cough or sneeze and throw the tissue in the trash after you use it.
- Wash your hands often with soap and water. If not available, use an alcohol-based hand rub.
- Avoid touching your eyes, nose and mouth. Germs spread this way.
- Clean and disinfect surfaces and objects that may be contaminated with germs like the flu.
Thursday, December 21, 2017
KentuckyOne in negotiations for sale of major Louisville facilities; selling St. Joseph Martin to Appalachian Regional Healthcare
KentuckyOne announced Dec. 19 that it had signed a letter of intent with Appalachian Regional Healthcare to negotiate the sale of Saint Joseph Martin, a 25-bed critical-access hospital in Floyd County.
"We are pleased to be talking with this organization to guide the future of care for this unique community,” Kathy Stumbo, president of St. Joseph Martin, said in a news release. “ARH knows this community and has the experience and insight to continue improvements and investments to support patients, physicians, employees and all in this region.”
ARH is a not-for-profit health system that serves Eastern Kentucky and southern West Virginia. It operates 11 hospitals and several other health facilities. It is the largest provider of care and the single largest employer in southeastern Kentucky and the third largest private employer in southern West Virginia, according to the release.
On the same day, KentuckyOne and its parent company, Catholic Health Initiatives, announced that they had entered into"exclusive negotiations" with BlueMountain Capital Management, a New York-based hedge fund, for the sale of some of their Louisville facilities, according to a separate news release.
KentuckyOne announced in May that it planned to sell most of its hospitals and provider facilities. The Courier Journal reported: "Besides Jewish, its flagship hospital, the health system will sell Frazier Rehab Institute; Sts. Mary & Elizabeth Hospital; Medical Centers Jewish East, South, Southwest and Northeast; Jewish Hospital Shelbyville; Saint Joseph Martin and KentuckyOne Health Medical Group provider practices in Louisville and Martin."
The sales would leave KentuckyOne with this footprint: Our Lady of Peace, a behavioral-treatment hospital in Louisville, Flaget Memorial Hospital in Bardstown, Saint Joseph Hospital and Saint Joseph East in Lexington, Saint Joseph Jessamine in Nicholasville, Saint Joseph Mount Sterling, Saint Joseph London and Saint Joseph Berea, and affiliated provider practices.
KentuckyOne notes that the negotiations have just begun and that any transactions would be subject to due diligence and regulatory approvals. Both sets of negotiations are expected to continue over the coming months, says the releases.
Wednesday, December 20, 2017
GOP senator pre-files bill to raise cigarette tax by $1, use money to pay for Medicaid treatment of tobacco-related illnesses
 |
| Sen. Stephen Meredith |
The bill would create a $1 "health care reimbursement assessment" on every pack of cigarettes sold in Kentucky, raising the total tax to $1.60 per pack. The average state cigarette tax is $1.71. The tax would make parallel increases in other tobacco taxes.
The bill calls for 90 percent of the money to go to a reimbursement fund for Medicaid treatment of tobacco-related illnesses. The remaining 10 percent would fund tobacco-cessation programs in counties that have comprehensive smoke-free ordinances.
The bill says, "Amounts deposited in the fund shall not be used for expansion of the Medicaid program . . . and shall not be appropriated or transferred by the General Assembly for any other purposes."
Meredith told Spectrum News, “What I’m trying to do through this bill is recognize that people have the right to smoke. I don’t begrudge them that, but don’t ask me to pay for your health-care costs whenever you incur those illnesses that you know you’re going to have. It’s created a tremendous financial burden, I think, for our state.”
Kentucky has the nation's second highest adult and youth smoking rates, 24.5 and 17 percent. It also has the highest cancer death rate, and 34 percent of those deaths are related to smoking. Smoking-related health costs in Kentucky have been estimated at $1.92 billion a year.
“Everybody’s got an aversion to taxes,” he said. “That’s why we’ve had difficulty getting this done in the past. All I’m doing is asking people to be responsible, be accountable for your own health and don’t ask non-smokers to pay for your health care in the future if you’re going to choose to do this.”
Meredith's bill drew favorable comments from key legislators on the Dec. 18 "Kentucky Tonight" on KET. "I see it not so much as an increase in taxes but an increase in the user fee," said Rep. Addia Wuchner, chair of the House Health and Human Services Committee. Her Senate counterpart, fellow Republican Julie Raque Adams, said she was interested in targeting Medicaid, partly because "We have very very high rates of smoking in the expansion population."
Raising the cigarette tax by at least $1 is a main objective of a newly formed coalition of more than 100 health-care, business, education and health-advocacy groups called Coalition for a Smoke-Free Tomorrow, staffed by the Foundation for a Healthy Kentucky. The groups have touted the tax as a public-health tool and a partial answer to the state's budget problems, without making any recommendations on how the money should be spent.
"It’s time to enact the proven measures that will reduce smoking and its related illnesses, reduced quality of life and massive health care expenditures in Kentucky," foundation President and CEO Ben Chandler wrote in an op-ed for Kentucky news outlets. "We can honor our tobacco heritage without allowing it to continue plaguing both our health and our economy. We urge you to contact your legislators and tell them you support a $1 tobacco tax increase because it’s a win-win-win for Kentucky."
Marijuana, tobacco and opioids will get different types of debate than in previous legislative sessions, lawmakers indicate
Legislators will debate what to do with drugs of several types when the General Assembly opens in Frankfort Tuesday, Jan. 2. And the debates may be different than in past sessions, if the discussion on the Dec. 18 "Kentucky Tonight" on KET is indicative.
The four lawmakers, including the two health committee chairs, indicated that the use of marijuana will be debated more openly than before, and even for recreational purposes, and that more action will be taken against the opioid epidemic.
"I think we’re gonna see a little bit of everything introduced," said Louisville Republican Julie Raque Adams, chair of the Senate Health and Welfare Committee. "I think we’re gonna see a recreational bill," in addition to legislation for medical marijuana.
"A lot of people across the state of Kentucky have told me they’re tired of talk" and want to see some votes on the issue, Adams said. "We’re gonna see a lot of testimony."
The four lawmakers, including the two health committee chairs, indicated that the use of marijuana will be debated more openly than before, and even for recreational purposes, and that more action will be taken against the opioid epidemic.
"I think we’re gonna see a little bit of everything introduced," said Louisville Republican Julie Raque Adams, chair of the Senate Health and Welfare Committee. "I think we’re gonna see a recreational bill," in addition to legislation for medical marijuana.
"A lot of people across the state of Kentucky have told me they’re tired of talk" and want to see some votes on the issue, Adams said. "We’re gonna see a lot of testimony."
When host Renee Shaw asked if efforts to legalize marijuana would have trouble because some see it as gateway drug, or if there might be less resistance because it is seen as less harmful than opioids, Democratic Rep. Chris Harris of Pike County indicated the latter.
"I think the time is coming in Kentucky for medical marijuana," he said, adding that he has an "open mind" on the issue.
Rep. Angie Hatton, D-Whitesburg, said "My constituents want to talk about it more than almost any other issue," and it offers the possibility of tax revenue. "We have to talk about it."
Rep. Addia Wuchner, R-Florence, chair of the House Health and Human Services Committee, was skeptical of medical marijuana. A registered nurse and former hospital administrator, she said more research is needed.
Harris said, "There is some track record in other states," and added, "It could help a certain group of people."
Wuchner said legislators are trying for a comprehensive approach to the opioid epidemic, and Adams said they need to discuss a holistic approach with alternative approaches to drugs as the first option for pain relief.
Adams said Kentuckians should expect to see some criminal-justice reforms aimed at steering violators into recovery rather than putting them behind bars. "The trend lines for incarceration are all going in the wrong direction," she said. "We have to be creative about this opioid problem."
Adams said she will introduce a bill to keep the state from pre-empting local smoking ordinances, which are now a focus of anti-smoking advocates because Republican Gov. Matt Bevin opposes a statewide smoking ban. The bill would ban any state limits on local smoking laws.
Adams, who favors a statewide ban, said proposals for it prompted calls for local control, and "We listened. This is a creative way for us to say, 'Hey, start doing it.'" She noted that a Senate-passed bill to ban tobacco at all Kentucky schools got nowhere in the House.
Hatton said tobacco control "needs to be local decision" because it is "a personal freedom issue for a lot of people." Harris agreed, saying smoking bans should be "a step-by-step process. We need to walk before we can run."
 |
| L-R: Reps. Angie Hatton, Chris Harris, Addia Wuchner; host Renee Shaw; Sen. Julie Raque Adams |
Rep. Addia Wuchner, R-Florence, chair of the House Health and Human Services Committee, was skeptical of medical marijuana. A registered nurse and former hospital administrator, she said more research is needed.
Harris said, "There is some track record in other states," and added, "It could help a certain group of people."
Wuchner said legislators are trying for a comprehensive approach to the opioid epidemic, and Adams said they need to discuss a holistic approach with alternative approaches to drugs as the first option for pain relief.
Adams said Kentuckians should expect to see some criminal-justice reforms aimed at steering violators into recovery rather than putting them behind bars. "The trend lines for incarceration are all going in the wrong direction," she said. "We have to be creative about this opioid problem."
Adams said she will introduce a bill to keep the state from pre-empting local smoking ordinances, which are now a focus of anti-smoking advocates because Republican Gov. Matt Bevin opposes a statewide smoking ban. The bill would ban any state limits on local smoking laws.
Adams, who favors a statewide ban, said proposals for it prompted calls for local control, and "We listened. This is a creative way for us to say, 'Hey, start doing it.'" She noted that a Senate-passed bill to ban tobacco at all Kentucky schools got nowhere in the House.
Hatton said tobacco control "needs to be local decision" because it is "a personal freedom issue for a lot of people." Harris agreed, saying smoking bans should be "a step-by-step process. We need to walk before we can run."
#SinkDiabetes campaign asks Kentuckians to shoot a trick shot to fight a disease that many in state have or are at risk of having
Shooting hoops to bring awareness and raise money for diabetes sounds like something Kentuckians could get excited about.
The Barnstable Brown Diabetes Center at the University of Kentucky says it has started a social-media campaign called #SinkDiabetes to bring awareness to a disease that affects more than 458,000 Kentuckians, or 13.4 percent of the population, more than the average state.
The campaign involves recording yourself taking a trick shot and posting it on social media with the hashtag #SinkDiabetes and tag three other people. For every #SinkDiabetes post, $10 will be donated to the diabetes center.
In addition, each person participating is asked to challenge – and tag – three more friends to participate in the #SinkDiabetes campaign. The campaign will run through the end of January.
The state's 2017 Kentucky Diabetes Fact Sheet calls the disease a "public health epidemic," adding that more than one-third of Kentuckians (37 percent) have a condition called pre-diabetes, which puts them at risk for the disease -- and most of them don't know it.
The Barnstable Brown Diabetes Center at the University of Kentucky says it has started a social-media campaign called #SinkDiabetes to bring awareness to a disease that affects more than 458,000 Kentuckians, or 13.4 percent of the population, more than the average state.
In addition, each person participating is asked to challenge – and tag – three more friends to participate in the #SinkDiabetes campaign. The campaign will run through the end of January.
The state's 2017 Kentucky Diabetes Fact Sheet calls the disease a "public health epidemic," adding that more than one-third of Kentuckians (37 percent) have a condition called pre-diabetes, which puts them at risk for the disease -- and most of them don't know it.
Tuesday, December 19, 2017
UK Markey Cancer Center gets outstanding achievement award
 |
Lucille Parker Markey Cancer Center at UK
|
The award is intended to recognize those cancer programs that achieve excellence meeting the commission's standards; motivate other cancer programs to work toward improving their level of quality cancer care; facilitate dialogue between award recipients and health care professionals at other cancer facilities for the purpose of sharing best practices; and encourage honorees to serve as quality care resources to other cancer programs, according to a University of Kentucky news release.
"I'm incredibly proud of the efforts our physicians, nurses, and other medical staff put in on a daily basis," Dr. Mark Evers, director of the center, said in the release. "This latest national award is another recognition of the hard work that goes on here, and the top-tier care we're able to offer patients from the Commonwealth and beyond."
Earlier this year, U.S. News & World Report named Markey one of the top 50 cancer programs in the nation. Additionally, Markey received a prestigious National Cancer Institute designation in 2013 and is up for renewal of this designation in 2018.
Sunday, December 17, 2017
HIV outbreak in Appalachian Ky. 'just a matter of time;' majority of counties CDC calls most vulnerable have no syringe exchange
An outbreak of the human immunodeficiency virus, which leads to AIDS, is “just a matter of time” in Appalachian Kentucky because of conditions in the region and the lack of syringe exchanges for intravenous drug users in most vulnerable counties.
That's what Dr. Jennifer Havens, an epidemiologist at the University of Kentucky, told the Courier Journal's Laura Ungar for a story updating the county-by-county threat first identified by the federal Centers for Disease Control and Prevention in 2016.
Using "statistics tied to injecting drugs, such as overdose deaths, prescription-opioid sales, low income and unemployment," Ungar notes, the CDC identified 220 counties in the U.S. that were most vulnerable to outbreaks of HIV or hepatitis C, a liver infection that can also be spread by needle sharing.
Kentucky has 54 of those counties, mostly in Eastern and Southern Kentucky, but 30 of them "haven’t given the go-ahead for needle exchanges," Ungar reports. "And programs approved in the vulnerable counties of Wolfe, Perry and Letcher have yet to open." Ungar's story has a national, interactive map with the ranking of each county.
 |
| Dr. Jennifer Havens |
Using "statistics tied to injecting drugs, such as overdose deaths, prescription-opioid sales, low income and unemployment," Ungar notes, the CDC identified 220 counties in the U.S. that were most vulnerable to outbreaks of HIV or hepatitis C, a liver infection that can also be spread by needle sharing.
Kentucky has 54 of those counties, mostly in Eastern and Southern Kentucky, but 30 of them "haven’t given the go-ahead for needle exchanges," Ungar reports. "And programs approved in the vulnerable counties of Wolfe, Perry and Letcher have yet to open." Ungar's story has a national, interactive map with the ranking of each county.
Ungar adds, "Elizabeth Turner, director of the district health department covering those counties, said they’ve managed to partly fund Wolfe’s exchange but are having trouble buying needles because some of the grant money can’t be used for them. She explained the situation to a state health official this week, she said, and was told Kentucky just received harm reduction funds that will be sent out to counties, including Wolfe. Although this money also can't be used for needles, Turner is hopeful it could offset other expenses," freeing up money to buy syringes.
"HIV has been found across Appalachia, though known
rates so far are lower than in urban Kentucky, where testing is more
common," Ungar reports. "April Young, a University of Kentucky assistant professor of
epidemiology, said less HIV testing in Eastern Kentucky means the
disease could be spreading silently."
As evidence of that, "Researchers point to an explosion of HIV’s widely-accepted harbinger: the potentially deadly liver disease hepatitis C," Ungar notes. "Like
HIV, 'hep C' can be spread by sharing needles. And it’s easier to
contract, so it’s not uncommon to have both diseases. . . . Havens’ long-term study of Eastern Kentucky drug users found that once they start shooting up, most get hep C within a year. . . . From 2008 to 2015, Kentucky had the nation's highest rate of new, acute hep C infections, with 1,089 cases. Another 38,000 Kentuckians live with chronic
hep C. "
Meanwhile, “People have forgotten about HIV. … But it’s becoming
clear you have the stage set for a major increase in these infections
(in places) we’ve basically ignored,” Dr. Paul Volberding, director
of the AIDS Research Institute at the University of California-San Francisco, told Ungar. “Whenever we have an infectious disease and we turn our back,
it bites us.”
Ungar writes, “Many believe the solution begins
with fighting addiction in each family, school and community. But the
sheer scope of the drug scourge dwarfs grassroots efforts."
Medicaid expansion had much bigger impact in rural areas; advocates worry about impact of tax bill on programs
By Melissa Patrick
Kentucky Health News
The expansion of Medicaid under the Patient Protection and Affordable Care Act resulted in larger coverage gains in rural areas than urban ones, suggesting that any roll-back of the program would hurt rural America the most, according to a recent University of Louisville study.
The study, published in The Journal of Rural Health, found the percentage of low-income residents who signed up for health insurance through the expansion was greater in rural regions compared to urban ones: an 8.5 percent increase, compared to a 4.1 percent increase, respectively.
These findings are especially important to Kentucky, which had more rural people sign up for Medicaid through the expansion of the program to people who earn up to 138 percent of the federal poverty level than any other state, according to the Kentucky Center for Economic Policy.
In all, 478,000 Kentuckians signed up for coverage through the expansion and 223,700 of them lived in rural areas. Medicaid as a whole covers about 1.4 million Kentuckians. For a spreadsheet of enrollment by county in June 2017, click here.
The U of L researchers used data from the 2011-2015 Behavioral Risk Factor Surveillance System and compared trend changes for coverage, access to care and health care utilization in response to Medicaid expansion among urban and rural residents.
Joseph Benitez, who led the study as an assistant professor in U of L's School of Public Health and Information Sciences, said that even with the Medicaid expansion, cost-related barriers weighed more heavily on rural residents related to things like transportation to a medical provider. He said that can be problematic for individuals who live in health provider shortage areas.
“Any efforts by the government to roll back Medicaid expansion will certainly disproportionately affect the ability of rural residents to gain affordable coverage and access to care,” Benitez said in a news release.
Health advocates fear impact of tax cuts
While there isn't much talk right now about repealing and replacing the Affordable Care Act, the tax bill that is about to become law could trigger cuts to Medicaid funding down the line to help reduce the deficit most economists expect it to create.
Janet Currie, chair of the economics department at Princeton University and co-director of the Center for Health and Wellbeing, told Daniel Bush of "PBS NewsHour" that potential cuts to Medicare and Medicaid are "by far the most important potential impact of the tax bill on the health-care system. A $1.5 trillion (or larger) deficit will necessitate spending cuts. And cutting large social programs like Medicare and Medicaid using across the board cuts is the absolute worse way to do it."
Medicaid is jointly funded by the federal government and states, with the payment mix for traditional coverage varying depending on how poor the state is. For example, the federal government pays an average of 57 percent of traditional Medicaid costs, but pays 70 percent of the costs in Kentucky.
Medicaid expansion is paid at a higher rate. The federal government paid the full amount of the expansion until 2016; states are paying 5 percent of the cost this year, rising in steps to the law's maximum of 10 percent in 2020.
Kentucky Health News
The expansion of Medicaid under the Patient Protection and Affordable Care Act resulted in larger coverage gains in rural areas than urban ones, suggesting that any roll-back of the program would hurt rural America the most, according to a recent University of Louisville study.
The study, published in The Journal of Rural Health, found the percentage of low-income residents who signed up for health insurance through the expansion was greater in rural regions compared to urban ones: an 8.5 percent increase, compared to a 4.1 percent increase, respectively.
These findings are especially important to Kentucky, which had more rural people sign up for Medicaid through the expansion of the program to people who earn up to 138 percent of the federal poverty level than any other state, according to the Kentucky Center for Economic Policy.
In all, 478,000 Kentuckians signed up for coverage through the expansion and 223,700 of them lived in rural areas. Medicaid as a whole covers about 1.4 million Kentuckians. For a spreadsheet of enrollment by county in June 2017, click here.
The U of L researchers used data from the 2011-2015 Behavioral Risk Factor Surveillance System and compared trend changes for coverage, access to care and health care utilization in response to Medicaid expansion among urban and rural residents.
“Any efforts by the government to roll back Medicaid expansion will certainly disproportionately affect the ability of rural residents to gain affordable coverage and access to care,” Benitez said in a news release.
Health advocates fear impact of tax cuts
While there isn't much talk right now about repealing and replacing the Affordable Care Act, the tax bill that is about to become law could trigger cuts to Medicaid funding down the line to help reduce the deficit most economists expect it to create.
Janet Currie, chair of the economics department at Princeton University and co-director of the Center for Health and Wellbeing, told Daniel Bush of "PBS NewsHour" that potential cuts to Medicare and Medicaid are "by far the most important potential impact of the tax bill on the health-care system. A $1.5 trillion (or larger) deficit will necessitate spending cuts. And cutting large social programs like Medicare and Medicaid using across the board cuts is the absolute worse way to do it."
Medicaid is jointly funded by the federal government and states, with the payment mix for traditional coverage varying depending on how poor the state is. For example, the federal government pays an average of 57 percent of traditional Medicaid costs, but pays 70 percent of the costs in Kentucky.
Medicaid expansion is paid at a higher rate. The federal government paid the full amount of the expansion until 2016; states are paying 5 percent of the cost this year, rising in steps to the law's maximum of 10 percent in 2020.
New 'bridge clinics' at UK and Northern Kentucky link emergency care to opioid-addiction treatment; U of L will also have one
Patients with opioid addictions who are treated in emergency rooms at the University of Kentucky or St. Elizabeth Hospital in Northern Kentucky can now go directly into addiction treatment if they choose it.
"An essential part of the substance-use-disorder treatment system is to be able provide treatment on demand rather than sending patients who are at risk for overdose death to treatment waiting lists," Dr. Laura Fanucchi, one of the creators of the clinic, said in a UK news release. "This way we can engage patients and link to treatment at the moment of contact with the health care system, and hopefully reduce substance use related morbidity and mortality."
The First Bridge Clinic, located at the UK Center on Drug and Alcohol Research, is set up to provide evidence-based care including medications approved by the U.S. Food and Drug Administration "for opioid-use disorder, counseling services, and monitoring aimed to promote remission and recovery," says the release.
UK's "bridge clinic" is one of three that are part of a project to fight opioid abuse in the state, funded by a nearly $10.5 million 21st Century CURES Act grant that is earmarked to be spent on a combination of evidence-based projects that focus on prevention, treatment and harm reductions.
St. Elizabeth opened the second bridge clinic at its Edgewood hospital in October and is working to expand its services to other St. Elizabeth hospitals, Terry DeMio reports for The Cincinnati Enquirer. The third one will be affiliated with the University of Louisville Hospital.
The news release says that after being awarded the grant, the state began to look for ideas to address the opioid epidemic and Drs. Sharon Walsh, Michelle Lofwall and Laura Fanucchi submitted a plan to make hospital emergency departments a first point of treatment for people with addictions.
“We’re developing a new clinic and it’s going to partner closely with the ED so when patients are referred they can receive care rapidly and within the same health care system with the aid of peer support,” Walsh said in the release.
Patients with opioid-use disorders end up in an emergency room for a variety of reasons, whether it be an overdose or a "deep-seated infection" related to their injection sites. Until now, such patients would be treated for their overdose or medical condition, but would not receive care for their underlying substance disorder.
"The need for this clinic is clear," Lofwall said in the release. “If the underlying addiction isn’t treated the person goes back to active addiction and is at very high risk for death and/or reinfection requiring another hospitalization with complicated medical and surgical treatments.”
"An essential part of the substance-use-disorder treatment system is to be able provide treatment on demand rather than sending patients who are at risk for overdose death to treatment waiting lists," Dr. Laura Fanucchi, one of the creators of the clinic, said in a UK news release. "This way we can engage patients and link to treatment at the moment of contact with the health care system, and hopefully reduce substance use related morbidity and mortality."
UK's "bridge clinic" is one of three that are part of a project to fight opioid abuse in the state, funded by a nearly $10.5 million 21st Century CURES Act grant that is earmarked to be spent on a combination of evidence-based projects that focus on prevention, treatment and harm reductions.
St. Elizabeth opened the second bridge clinic at its Edgewood hospital in October and is working to expand its services to other St. Elizabeth hospitals, Terry DeMio reports for The Cincinnati Enquirer. The third one will be affiliated with the University of Louisville Hospital.
The news release says that after being awarded the grant, the state began to look for ideas to address the opioid epidemic and Drs. Sharon Walsh, Michelle Lofwall and Laura Fanucchi submitted a plan to make hospital emergency departments a first point of treatment for people with addictions.
“We’re developing a new clinic and it’s going to partner closely with the ED so when patients are referred they can receive care rapidly and within the same health care system with the aid of peer support,” Walsh said in the release.
Patients with opioid-use disorders end up in an emergency room for a variety of reasons, whether it be an overdose or a "deep-seated infection" related to their injection sites. Until now, such patients would be treated for their overdose or medical condition, but would not receive care for their underlying substance disorder.
"The need for this clinic is clear," Lofwall said in the release. “If the underlying addiction isn’t treated the person goes back to active addiction and is at very high risk for death and/or reinfection requiring another hospitalization with complicated medical and surgical treatments.”
Pilot project will target men in the workplace in eight Kentucky counties, in an effort to prevent lung cancer
Eight Kentucky counties have been chosen to be part of a pilot program that will target males in the workplace to decrease lung cancer in the state, Renee Beasley Jones
reports for The Messenger-Inquirer in Owensboro.
"Kentucky has the highest rate of new cases and deaths from lung cancer in the nation, and in many counties throughout Kentucky, the rates are significantly higher in males than females," Jennifer Redmond Knight, assistant professor of health management and policy at the University of Kentucky College of Public Health, told Jones.
The eight counties are Casey, Christian, Clay, Jackson, McCracken, Ohio, Perry and Warren. Jones writes that they were chosen based on their rates of lung cancer, poverty status, whether they were considered medically under-served, had low levels of literacy and high rates of hospitalizations.
The project is funded by the Centers for Disease Control and Prevention's SelfMade Health Network, which works toward tobacco and cancer prevention efforts in populations that have high disparities of both.
The pilot is targeting men in workplaces because they have "significantly higher rates" of cancer and deaths from lung cancer, and because the Kentucky Cancer Program has learned through experience that one of the best ways to reach men with health-related information is at work, Jennifer Redmond Knight, who is also the lead investigator, told Jones.
She added that the goals of the program include: reducing the smoking rate, increasing the number of radon tests conducted in homes, reducing the number of people exposed to secondhand smoke and increasing lung-cancer screenings. The ultimate goal is to reduce lung cancer rates in Kentucky.
Radon,which is an odorless, colorless and tasteless gas, is the second leading cause of lung cancer and studies show that the combination of radon gas and cigarette smoke increases the risk for lung cancer more than either factor alone. Click here for more information about radon and to learn how to get a free radon test kit.
The pilot program will eventually develop a lung cancer work site resource kit, based on feedback from participating businesses, that can be used across the state. The pilot is expected to go through January 2019.
Jones writes that six businesses in Ohio County are participating in the program including Perdue Foods, which has an extensive wellness program. Angie Hudnall, the plant's RN health improvement program specialist, told Jones that the pilot program complements their plant's health improvement program.
She said: "The pilot program matches our focus on primary care, prevention and early intervention to improve associate health and reduce health-care costs -- for our associates and for our company."
"Kentucky has the highest rate of new cases and deaths from lung cancer in the nation, and in many counties throughout Kentucky, the rates are significantly higher in males than females," Jennifer Redmond Knight, assistant professor of health management and policy at the University of Kentucky College of Public Health, told Jones.
The eight counties are Casey, Christian, Clay, Jackson, McCracken, Ohio, Perry and Warren. Jones writes that they were chosen based on their rates of lung cancer, poverty status, whether they were considered medically under-served, had low levels of literacy and high rates of hospitalizations.
The project is funded by the Centers for Disease Control and Prevention's SelfMade Health Network, which works toward tobacco and cancer prevention efforts in populations that have high disparities of both.
 |
| Kentucky Cancer Registry maps show lung cancer incidence and mortality rates for men in Kentucky between 2010 and 2014. Second map highlights Casey County. |
The program, called Lung Cancer Prevention and Survivorship Is Good Business, will target businesses where more than half the employees are men. It will be coordinated by the College of Public Health, the Kentucky Cancer Program and the Kentucky Cancer Consortium.
She added that the goals of the program include: reducing the smoking rate, increasing the number of radon tests conducted in homes, reducing the number of people exposed to secondhand smoke and increasing lung-cancer screenings. The ultimate goal is to reduce lung cancer rates in Kentucky.
Radon,which is an odorless, colorless and tasteless gas, is the second leading cause of lung cancer and studies show that the combination of radon gas and cigarette smoke increases the risk for lung cancer more than either factor alone. Click here for more information about radon and to learn how to get a free radon test kit.
The pilot program will eventually develop a lung cancer work site resource kit, based on feedback from participating businesses, that can be used across the state. The pilot is expected to go through January 2019.
Jones writes that six businesses in Ohio County are participating in the program including Perdue Foods, which has an extensive wellness program. Angie Hudnall, the plant's RN health improvement program specialist, told Jones that the pilot program complements their plant's health improvement program.
She said: "The pilot program matches our focus on primary care, prevention and early intervention to improve associate health and reduce health-care costs -- for our associates and for our company."
Saturday, December 16, 2017
10 states gave Medicaid clients incentives for prevention; Ky. was not among them, but pending waiver would include one
Under the Patient Protection and Affordable Care Act, 10 states participated in a program that offered incentives to Medicaid clients if they engaged in targeted efforts to prevent chronic disease.
Patricia Alexander of California was a recipient of one of those incentives, which prompted her to get a mammogram. She told Anna Gorman of Kaiser Health News that every time she made an appointment, something came up, and it wasn't until her doctor's office promised her a $25 Target gift card that she was motivated to make the appointment and keep it. The mammogram was negative for breast cancer, but not all mammograms are.
Other states participating in the five-year demonstration projects were Connecticut, Hawaii, Minnesota, Montana, Nevada, New Hampshire, New York, Texas and Wisconsin. In all, they were awarded grants totaling $85 million, Gorman reports.
The practice of offering rewards as a motivation for patients to engage in more preventive care and to make healthier lifestyle choices has long been a practice of private health plans and the demonstration project was created to see if this practice would also work with the Medicaid population.
The states used the incentives for a variety of programs including ones to encourage people to enroll in diabetes prevention, weight management, smoking cessation and other preventive programs.
For example, California's program offered gift cards and nicotine replacement therapy to people who called the state's smoking cessation line and Minnesota's program gave cash to people who attended a diabetes prevention class and completed bloodwork, Gorman reports.
An evaluation of these programs, released in April, found that the incentives helped persuade the Medicaid beneficiaries to participate in preventive activities, but it wasn't able to show that the programs prevented chronic disease or save Medicaid money. The report noted that this was largely because the prevention of chronic diseases could take years to manifest.
Gorman reports that research on the effectiveness of financial incentives for the Medicaid population has been mixed.
She also points to a report released this year by the liberal-leaning Center on Budget and Policy Priorities that found incentives were good to change immediate behaviors like keeping a doctor's appointment or attending a class, but were less likely to change long-term behaviors, like weight loss.
“The thing that is most likely to help Medicaid beneficiaries utilize care appropriately is actually just giving them access to that care — and that includes providing transportation and child care,” Hannah Katch, an author of the center's report, told Gorman. She added that another barrier is being able to take time off work to go to the doctor.
The report says that these types of incentive programs have proven to pose administrative challenges as well as provider engagement and participation challenges. In addition, it says patient and provider education about the programs; identifying and engaging beneficiaries to participate; establishing the infrastructure to offer and provide the incentives; and the added costs to states to implement these programs have all provided challenges to such programs.
A huge motivator to these incentives programs is to help clients become healthier because insurers "know they can reduce their costs -- and increase their profits -- if their patients are healthier," Gorman writes.
Doug Hogan, spokesman for Kentucky's Cabinet for Health and Family Services, said the state doesn't have such an incentive program for its Medicaid beneficiaries, but if federal officials approve its new Medicaid program, which state officials call Kentucky HEALTH, it will have incentives to encourage members to improve their health and be active members of the community.
"The program would do so by offering My Rewards dollars for activities like accessing preventive-care services, taking health and financial literacy classes, and participating in job training programs," Hogan said. "Members can then use the dollars to access some services not covered by the Kentucky HEALTH plan. Furthermore, members can receive up to $500 from their My Rewards account once they transition to a commercial insurance plan for at least 18 months."
Gov. Matt Bevin proposed changes to Kentucky Medicaid by requesting a waiver from federal rules more than a year ago. The proposal largely targets "able-bodied" adults who qualify for Medicaid under the ACA's expansion of the program to those who earn up to 138 percent of the federal poverty level. It is expected to be approved.
Patricia Alexander of California was a recipient of one of those incentives, which prompted her to get a mammogram. She told Anna Gorman of Kaiser Health News that every time she made an appointment, something came up, and it wasn't until her doctor's office promised her a $25 Target gift card that she was motivated to make the appointment and keep it. The mammogram was negative for breast cancer, but not all mammograms are.
Other states participating in the five-year demonstration projects were Connecticut, Hawaii, Minnesota, Montana, Nevada, New Hampshire, New York, Texas and Wisconsin. In all, they were awarded grants totaling $85 million, Gorman reports.
The practice of offering rewards as a motivation for patients to engage in more preventive care and to make healthier lifestyle choices has long been a practice of private health plans and the demonstration project was created to see if this practice would also work with the Medicaid population.
The states used the incentives for a variety of programs including ones to encourage people to enroll in diabetes prevention, weight management, smoking cessation and other preventive programs.
For example, California's program offered gift cards and nicotine replacement therapy to people who called the state's smoking cessation line and Minnesota's program gave cash to people who attended a diabetes prevention class and completed bloodwork, Gorman reports.
An evaluation of these programs, released in April, found that the incentives helped persuade the Medicaid beneficiaries to participate in preventive activities, but it wasn't able to show that the programs prevented chronic disease or save Medicaid money. The report noted that this was largely because the prevention of chronic diseases could take years to manifest.
Gorman reports that research on the effectiveness of financial incentives for the Medicaid population has been mixed.
She also points to a report released this year by the liberal-leaning Center on Budget and Policy Priorities that found incentives were good to change immediate behaviors like keeping a doctor's appointment or attending a class, but were less likely to change long-term behaviors, like weight loss.
“The thing that is most likely to help Medicaid beneficiaries utilize care appropriately is actually just giving them access to that care — and that includes providing transportation and child care,” Hannah Katch, an author of the center's report, told Gorman. She added that another barrier is being able to take time off work to go to the doctor.
The report says that these types of incentive programs have proven to pose administrative challenges as well as provider engagement and participation challenges. In addition, it says patient and provider education about the programs; identifying and engaging beneficiaries to participate; establishing the infrastructure to offer and provide the incentives; and the added costs to states to implement these programs have all provided challenges to such programs.
A huge motivator to these incentives programs is to help clients become healthier because insurers "know they can reduce their costs -- and increase their profits -- if their patients are healthier," Gorman writes.
Doug Hogan, spokesman for Kentucky's Cabinet for Health and Family Services, said the state doesn't have such an incentive program for its Medicaid beneficiaries, but if federal officials approve its new Medicaid program, which state officials call Kentucky HEALTH, it will have incentives to encourage members to improve their health and be active members of the community.
"The program would do so by offering My Rewards dollars for activities like accessing preventive-care services, taking health and financial literacy classes, and participating in job training programs," Hogan said. "Members can then use the dollars to access some services not covered by the Kentucky HEALTH plan. Furthermore, members can receive up to $500 from their My Rewards account once they transition to a commercial insurance plan for at least 18 months."
Gov. Matt Bevin proposed changes to Kentucky Medicaid by requesting a waiver from federal rules more than a year ago. The proposal largely targets "able-bodied" adults who qualify for Medicaid under the ACA's expansion of the program to those who earn up to 138 percent of the federal poverty level. It is expected to be approved.
Bevin's lawsuit against Planned Parenthood revived
The Kentucky Court of Appeals has reinstated Gov. Matt Bevin's lawsuit that claims Planned Parenthood of Indiana and Kentucky illegally provided 23 abortions at its Louisville clinic.
Steve Pitt, Bevin's general counsel, said in a statement: “The facts are clear and alarming: Between Dec. 3, 2015 and Jan. 28, 2016, Planned Parenthood’s Louisville facility performed 23 abortions without proper licensing or emergency safeguards in place.” The Bevin administration is seeking fines of more than $500,000, the newspaper reports.
Steve Pitt, Bevin's general counsel, said in a statement: “The facts are clear and alarming: Between Dec. 3, 2015 and Jan. 28, 2016, Planned Parenthood’s Louisville facility performed 23 abortions without proper licensing or emergency safeguards in place.” The Bevin administration is seeking fines of more than $500,000, the newspaper reports.
A Louisville judge had dismissed the case in July, finding that "Planned Parenthood had been following directions of state officials when it began offering abortions in December as part of its effort to obtain a state license," the Courier Journal reported then.
The unanimous Dec. 15 ruling by a three-judge Court of Appeals panel said, "While the Cabinet [for Health and Family Services] may have a difficult time proving its allegations, we believe said allegations are sufficient to state a claim upon which relief can be granted." The trial judge had said the charges were insufficient.
“As the ruling states, this decision is not a statement on the merits of the case,” Christie Gillespie, President and CEO of the Planned Parenthood unit, said in a statement. “PPINK sought the advice of the governmental agency charged with overseeing licensure and followed its guidance. We did nothing wrong, and we are confident the courts will agree. We are committed to providing high-quality health care for all at our Kentucky health centers, and we will continue to do so while this case is litigated.”
“As the ruling states, this decision is not a statement on the merits of the case,” Christie Gillespie, President and CEO of the Planned Parenthood unit, said in a statement. “PPINK sought the advice of the governmental agency charged with overseeing licensure and followed its guidance. We did nothing wrong, and we are confident the courts will agree. We are committed to providing high-quality health care for all at our Kentucky health centers, and we will continue to do so while this case is litigated.”
Wednesday, December 13, 2017
States use only 3 percent of tobacco revenue for tobacco prevention, and Kentucky spends even less: 0.7 percent
When cigarette manufacturers agreed in 1998 to pay billions of dollars to settle a lawsuit by states seeking reimbursement of health costs related to smoking, the presumption was that the states would spend a large part of the money on tobacco prevention. Few have, and Kentucky is among the low spenders, though it is a national leader in smoking and tobacco-related health costs.
Those points are made annually in reports by the Campaign for Tobacco-Free Kids, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Robert Wood Johnson Foundation and the Americans for Nonsmokers' Rights and Truth Initiative.
The latest report, "Broken Promises to Our Children: A State-by-State Look at the 1998 Tobacco Settlement 19 Years Later," says states will spend less than 3 percent of this fiscal year's settlement funds and tobacco taxes – $27.5 billion out of $721.6 million – "on programs to prevent kids from smoking and help smokers quit."
The report says Kentucky will get $371 million this fiscal year from the settlement and tobacco taxes, but will spend only $2.6 million on tobacco prevention, a meager 0.7 percent. The spending is less than 5 percent of the $56 million that the federal Centers for Disease Control and Prevention says the state should spend.
Ben Chandler, president and CEO of the foundation, said "Kentucky continues to make small strides in reducing smoking rates among both adults and youth, but we remain substantially higher than the national average and almost every other state. That's particularly true in Appalachian counties, where the rate hovers around 30 percent, double the national average. The single most effective way to reduce these rates is to raise the price of cigarettes through a substantial state tax increase of at least $1 per pack."
Those points are made annually in reports by the Campaign for Tobacco-Free Kids, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Robert Wood Johnson Foundation and the Americans for Nonsmokers' Rights and Truth Initiative.
The latest report, "Broken Promises to Our Children: A State-by-State Look at the 1998 Tobacco Settlement 19 Years Later," says states will spend less than 3 percent of this fiscal year's settlement funds and tobacco taxes – $27.5 billion out of $721.6 million – "on programs to prevent kids from smoking and help smokers quit."
The report says Kentucky will get $371 million this fiscal year from the settlement and tobacco taxes, but will spend only $2.6 million on tobacco prevention, a meager 0.7 percent. The spending is less than 5 percent of the $56 million that the federal Centers for Disease Control and Prevention says the state should spend.
Meanwhile, tobacco companies spend $250 million a year on marketing in Kentucky, and $8.9 billion nationally – "$1 million every hour – to market their deadly and addictive products," the report says.
That's way out of whack, said Charlie Ross of Mayfield, board chair of the Foundation for a Healthy Kentucky. "Health care expenses and productivity losses tied to smoking total more than $19 per pack, yet the state gets just 60 cents per pack in tobacco taxes," Ross said in a release. "It seems pretty straightforward that we need to focus more resources on preventing what's behind these costs. We'll not only reduce health-care expenditures, we'll save lives and draw more jobs to the Commonwealth from companies that need a healthy workforce to grow their business."
Ben Chandler, president and CEO of the foundation, said "Kentucky continues to make small strides in reducing smoking rates among both adults and youth, but we remain substantially higher than the national average and almost every other state. That's particularly true in Appalachian counties, where the rate hovers around 30 percent, double the national average. The single most effective way to reduce these rates is to raise the price of cigarettes through a substantial state tax increase of at least $1 per pack."
Tuesday, December 12, 2017
Kentucky ranked 42nd in America's Health Rankings this year, up from 45th last year, but there's little to celebrate
Kentucky moved up three notches in the latest America's Health Rankings, from 45th to 42nd, but its improvement stemmed mainly from gains in the factors that determine health, not the actual health outcomes. The state was 39th in health determinants (clinical care, policy, community and environment) but 46th in outcomes, such as the death rate from cancer, which is the nation's worst.
That was reflected in the rankings of behaviors, such as the smoking rate and the rate of drug deaths, both second largest in the nation, as well as obesity and physical inactivity. But the behavior score was helped by a high rate of high-school graduation and a low rate of excessive drinking.
The state's highest rankings came in health policy. It was ninth in the nation in the percentage of residents covered by health insurance, thanks to its expansion of Medicaid under the Patient Protection and Affordable Care Act. It also ranked better than average in some measures of community and environment, such as infectious diseases.
"Kentucky made progress in some areas, including expanding the number of residents with health insurance, but drug deaths are up dramatically, and our high rate of obesity remains a challenge," said Ben Chandler, president and CEO of the Foundation for a Healthy Kentucky. "Our high smoking rate is a plague we know how to address, however. It's a huge contributing factor to our ranking as the cancer capital of the nation and our inability to reduce low birth-weight babies, heart disease and premature death. Smoking rates declined 2 percent nationally since last year, but only 1.4 percentage points in Kentucky. Raising the tobacco tax by at least $1 and enacting more smoke-free laws in counties and cities across the Commonwealth are two measures that will kick-start a greater decline in smoking rates and better health."
Since the rankings were first released in 1990, with the exception of 2008 when it ranked 39th, Kentucky has ranked in the bottom 10 states for health. It was 44th in 2010, 43rd in 2011, 44th in 2012, 45th in 2013, 47th in 2014, 44th in 2015, and 45th in 2016. Here are this year's figures:
That was reflected in the rankings of behaviors, such as the smoking rate and the rate of drug deaths, both second largest in the nation, as well as obesity and physical inactivity. But the behavior score was helped by a high rate of high-school graduation and a low rate of excessive drinking.
The state's highest rankings came in health policy. It was ninth in the nation in the percentage of residents covered by health insurance, thanks to its expansion of Medicaid under the Patient Protection and Affordable Care Act. It also ranked better than average in some measures of community and environment, such as infectious diseases.
"Kentucky made progress in some areas, including expanding the number of residents with health insurance, but drug deaths are up dramatically, and our high rate of obesity remains a challenge," said Ben Chandler, president and CEO of the Foundation for a Healthy Kentucky. "Our high smoking rate is a plague we know how to address, however. It's a huge contributing factor to our ranking as the cancer capital of the nation and our inability to reduce low birth-weight babies, heart disease and premature death. Smoking rates declined 2 percent nationally since last year, but only 1.4 percentage points in Kentucky. Raising the tobacco tax by at least $1 and enacting more smoke-free laws in counties and cities across the Commonwealth are two measures that will kick-start a greater decline in smoking rates and better health."
Since the rankings were first released in 1990, with the exception of 2008 when it ranked 39th, Kentucky has ranked in the bottom 10 states for health. It was 44th in 2010, 43rd in 2011, 44th in 2012, 45th in 2013, 47th in 2014, 44th in 2015, and 45th in 2016. Here are this year's figures:
Sunday, December 10, 2017
We're in the final few days of open enrollment for insurance on healthcare.gov; automatic re-enrollment might not be the best way
Updated Dec. 11, 2017: This article has been edited to reflect that CareSource's marketplace products are not part of Humana.
By Melissa Patrick
Kentucky Health News
You have just a few days to enroll in a 2018 health-insurance plan on healthcare.gov. Open enrollment under the Patient Protection and Affordable Care Act ends Friday, Dec. 15.
"The clock is ticking," Whitney Allen, the outreach and enrollment coordinator for the Kentucky Primary Care Association, said in an e-mail. " We encourage anyone that has questions about enrolling in a 2018 health insurance plan to contact their local application assister before Dec. 15!"
And even if you don't need marketplace coverage, Allen says you should remind others, because that seems to be the way most people are hearing about government-subsidized insurance this year.
"It seems word of mouth has been the best advertising, this open enrollment," Allen said.
The state health agency has said it is using direct mail, text messages, phone calls and e-mails to communicate with current policyholders and potential new enrollees about open enrollment because it no longer gets federal funds for outreach.
Allen said most people in southeastern Kentucky who have called for application assistance say they heard about the service from family members and friends who have used it.
Who needs coverage?
Anyone who doesn't have health coverage through a job, Medicare, Medicaid, the Children's Health Insurance Program, or other coverage that meets federal standards, needs to sign up for marketplace coverage or risk paying a penalty.
The penalty for not having health insurance in 2018 is $695 per adult and $347.50 per child, with a maximum of $2,085 per family, or 2.5 percent of the household's income, whichever is larger.
If you miss the deadline, and don't qualify for a special enrollment period, you will have to wait another year to sign up, says the healthcare.gov website.
Health advocates have encouraged consumers to actively pick a plan to make sure they are getting the best coverage for the best cost, even if they will be automatically re-enrolled, as around 80,000 Kentuckians could be if they don't pick their own plan.
Stan Dorn, a senior fellow at Families USA, an advocacy group, told Kaiser Health News that auto-enrollment doesn't take premiums or benchmark plan changes into account, which means that even if you are assigned to the same plan, your cost could be different next year.
Kaiser Health News has also reported that it's important to actively choose a plan because "if you don't like the plan you're auto-enrollled in this year you may be stuck with it in 2018, unlike previous years when people could generally switch."
CareSource, which is offering exchange plans in 61 Kentucky counties, encouraged consumers to also check to see if their doctors are on their plans network.
"Even if a plan did not include your doctor last year, check again for 2018. Some plans, like CareSource, have recently signed agreements with new provider groups. This means more doctors may be in network beginning on January 1, 2018," CareSource said in a news release.
Anthem Blue Cross Blue Shield is selling plans in the other 59 counties. Here's a healthcare.gov checklist of the information that you need to have available when you sign up for coverage:
Where can I get help?
Application assisters are available in every Kentucky county to help people sign up for coverage, and their services are free. There are also sign-up events throughout the state. To find an event in your county or an assister, go to healthbenefitexchange.gov.
Help is also available through the state call center at 855-459-6328 and the Healthcare.gov customer center at 800-318-2596, which is available 24 hours a day, seven days a week.
Click here for a livestream open enrollment information session that aired Friday, Dec. 8 on the Kentuckians for The Commonwealth Facebook page. The video features application assisters from the Primary Care Association.
By Melissa Patrick
Kentucky Health News
You have just a few days to enroll in a 2018 health-insurance plan on healthcare.gov. Open enrollment under the Patient Protection and Affordable Care Act ends Friday, Dec. 15.
"The clock is ticking," Whitney Allen, the outreach and enrollment coordinator for the Kentucky Primary Care Association, said in an e-mail. " We encourage anyone that has questions about enrolling in a 2018 health insurance plan to contact their local application assister before Dec. 15!"
And even if you don't need marketplace coverage, Allen says you should remind others, because that seems to be the way most people are hearing about government-subsidized insurance this year.
"It seems word of mouth has been the best advertising, this open enrollment," Allen said.
The state health agency has said it is using direct mail, text messages, phone calls and e-mails to communicate with current policyholders and potential new enrollees about open enrollment because it no longer gets federal funds for outreach.
Allen said most people in southeastern Kentucky who have called for application assistance say they heard about the service from family members and friends who have used it.
Who needs coverage?
Anyone who doesn't have health coverage through a job, Medicare, Medicaid, the Children's Health Insurance Program, or other coverage that meets federal standards, needs to sign up for marketplace coverage or risk paying a penalty.
The penalty for not having health insurance in 2018 is $695 per adult and $347.50 per child, with a maximum of $2,085 per family, or 2.5 percent of the household's income, whichever is larger.
Health advocates have encouraged consumers to actively pick a plan to make sure they are getting the best coverage for the best cost, even if they will be automatically re-enrolled, as around 80,000 Kentuckians could be if they don't pick their own plan.
Stan Dorn, a senior fellow at Families USA, an advocacy group, told Kaiser Health News that auto-enrollment doesn't take premiums or benchmark plan changes into account, which means that even if you are assigned to the same plan, your cost could be different next year.
Kaiser Health News has also reported that it's important to actively choose a plan because "if you don't like the plan you're auto-enrollled in this year you may be stuck with it in 2018, unlike previous years when people could generally switch."
In general, the federal exchange plans are more attractive to individuals and families who earn less than 400 percent of the federal poverty level because they will qualify for subsidized coverage. And those who make too much to qualify for a subsidy are encouraged to connect with a certified health insurance agent or a broker to determine whether an exchange or off-exchange plan is best for them.
CareSource, which is offering exchange plans in 61 Kentucky counties, encouraged consumers to also check to see if their doctors are on their plans network.
"Even if a plan did not include your doctor last year, check again for 2018. Some plans, like CareSource, have recently signed agreements with new provider groups. This means more doctors may be in network beginning on January 1, 2018," CareSource said in a news release.
Anthem Blue Cross Blue Shield is selling plans in the other 59 counties. Here's a healthcare.gov checklist of the information that you need to have available when you sign up for coverage:
Where can I get help?
Application assisters are available in every Kentucky county to help people sign up for coverage, and their services are free. There are also sign-up events throughout the state. To find an event in your county or an assister, go to healthbenefitexchange.gov.
Help is also available through the state call center at 855-459-6328 and the Healthcare.gov customer center at 800-318-2596, which is available 24 hours a day, seven days a week.
Click here for a livestream open enrollment information session that aired Friday, Dec. 8 on the Kentuckians for The Commonwealth Facebook page. The video features application assisters from the Primary Care Association.
Friday, December 8, 2017
Flu and pneumonia, which can result from flu, are 8th largest U.S. cause of death; officials urge all over 6 months to get flu shot
Flu season is here and will last through February or longer, prompting state health officials to encourage Kentuckians to get their flu vaccinations.
“During the holidays families and friends will gather, which increases the potential for exposure to the flu virus," Dr. Jeffrey Howard, the state's acting health commissioner, said in a news release. "We urge everyone who hasn’t received the flu vaccine, particularly those at high risk for complications related to the flu, to check with their regular health care professional, local health departments or other vaccine providers.”
Flu is a "very contagious" disease caused by a virus that spreads from person to person. Symptoms include fever, headache, cough, sore throat, runny nose, sneezing and body aches.
It can also be deadly. Flu and pneumonia are the eighth leading causes of death in the United States, according to the federal Centers for Disease Control and Prevention.
Just this week, Jennifer Earl of CBS News reported that a 20-year-old mother of two in Arizona died unexpectedly and quickly from flu.
Alani "Joie" Murrieta of Phoenix was being treated for the flu with an anti-viral medication called Tamiflu, but her health took a turn for the worse the day after her diagnosis. She was then rushed to the hospital, diagnosed with pneumonia and started treatment, but within two days of when she started feeling ill she was dead.
“During the holidays families and friends will gather, which increases the potential for exposure to the flu virus," Dr. Jeffrey Howard, the state's acting health commissioner, said in a news release. "We urge everyone who hasn’t received the flu vaccine, particularly those at high risk for complications related to the flu, to check with their regular health care professional, local health departments or other vaccine providers.”
Flu is a "very contagious" disease caused by a virus that spreads from person to person. Symptoms include fever, headache, cough, sore throat, runny nose, sneezing and body aches.
It can also be deadly. Flu and pneumonia are the eighth leading causes of death in the United States, according to the federal Centers for Disease Control and Prevention.
Just this week, Jennifer Earl of CBS News reported that a 20-year-old mother of two in Arizona died unexpectedly and quickly from flu.
Alani "Joie" Murrieta of Phoenix was being treated for the flu with an anti-viral medication called Tamiflu, but her health took a turn for the worse the day after her diagnosis. She was then rushed to the hospital, diagnosed with pneumonia and started treatment, but within two days of when she started feeling ill she was dead.
Murrieta's aunt, Stephanie Gonzales, warned the public to take the flu seriously.
"Don't take life for granted. If you feel sick, go to the doctor. Don't wait until your symptoms are so bad there is no turning back," she told CBS.
Kentucky's flu level as of Friday was classified as "regional," with 104 laboratory-confirmed cases, according to the state's weekly influenza surveillance report. Twelve of the state's 17 regions have had a confirmed case this flu season. As of Dec. 2, there had been no flu-related deaths reported in Kentucky.
NPR reports that the flu season could be "unusually harsh" this year because of several factors.
One is this year's early start to the season, which could make it last longer and infect more people. Another is that Australia had a severe flu season this year and the U.S. typically has a similar experience to what happens in the southern hemisphere.
Australia's bad season stemmed from a strain of the flu virus called H3N2 that tends to make people sicker than other strains, and because the flu vaccine was only about 10 percent effective against that strain this year in Australia. The U.S. is using the same vaccine as Australia, but its effectiveness in the U.S. is still unknown.
Health experts say that even an imperfect vaccine is better than no vaccine because it can help prevent or lessen the severity of the illness and also helps to promote "herd immunity" of the population.
The CDC recommends that everyone over six months of age get a flu vaccination, and especially encourages people who may be at higher risk for complications or negative consequences get one. They include:
• Children age six months through 59 months;
• Women who are or will be pregnant during the influenza season;
• Persons 50 years of age or older;
• Persons with extreme obesity (body-mass index of 40 or greater);
• Persons aged six months and older with chronic health problems;
• Residents of nursing homes and other long-term care facilities;
• Household contacts (including children) and caregivers of children younger than 5, particularly contacts of such children, or of adults 50 and older;
• Household contacts and caregivers or people who live with a person at high-risk for complications from the flu; and
• Health care workers, including physicians, nurses, medical emergency-response workers, employees of nursing home and long-term care facilities who have contact with patients or residents, and students in these professions who will have contact with patients.
Howard added, “You should also follow the advice your parents gave you to prevent flu and other illnesses that tend to circulate at this time of year – wash your hands frequently, cover your mouth when you cough or sneeze and stay home when you’re sick.”
"Don't take life for granted. If you feel sick, go to the doctor. Don't wait until your symptoms are so bad there is no turning back," she told CBS.
Kentucky's flu level as of Friday was classified as "regional," with 104 laboratory-confirmed cases, according to the state's weekly influenza surveillance report. Twelve of the state's 17 regions have had a confirmed case this flu season. As of Dec. 2, there had been no flu-related deaths reported in Kentucky.
NPR reports that the flu season could be "unusually harsh" this year because of several factors.
One is this year's early start to the season, which could make it last longer and infect more people. Another is that Australia had a severe flu season this year and the U.S. typically has a similar experience to what happens in the southern hemisphere.
Australia's bad season stemmed from a strain of the flu virus called H3N2 that tends to make people sicker than other strains, and because the flu vaccine was only about 10 percent effective against that strain this year in Australia. The U.S. is using the same vaccine as Australia, but its effectiveness in the U.S. is still unknown.
Health experts say that even an imperfect vaccine is better than no vaccine because it can help prevent or lessen the severity of the illness and also helps to promote "herd immunity" of the population.
The CDC recommends that everyone over six months of age get a flu vaccination, and especially encourages people who may be at higher risk for complications or negative consequences get one. They include:
• Children age six months through 59 months;
• Women who are or will be pregnant during the influenza season;
• Persons 50 years of age or older;
• Persons with extreme obesity (body-mass index of 40 or greater);
• Persons aged six months and older with chronic health problems;
• Residents of nursing homes and other long-term care facilities;
• Household contacts (including children) and caregivers of children younger than 5, particularly contacts of such children, or of adults 50 and older;
• Household contacts and caregivers or people who live with a person at high-risk for complications from the flu; and
• Health care workers, including physicians, nurses, medical emergency-response workers, employees of nursing home and long-term care facilities who have contact with patients or residents, and students in these professions who will have contact with patients.
Howard added, “You should also follow the advice your parents gave you to prevent flu and other illnesses that tend to circulate at this time of year – wash your hands frequently, cover your mouth when you cough or sneeze and stay home when you’re sick.”
Wednesday, December 6, 2017
Groups pushing $1-a-pack increase in state cigarette tax make their sales pitch through an infographic
The group promoting a $1-a-pack increase in the state cigarette tax and local ordinances to ban smoking in workplaces has a new infographic to remind Kentuckians of the cost of smoking.
The graphic was created by Kentucky Voices for Health, part of the Coalition for a Smoke-Free Tomorrow, which says making the tax $1.60 per pack and raising other tobacco taxes would raise $266 million a year in revenue for the state. The average state cigarette tax is $1.71 per pack.
"Research shows that a tobacco tax increase in Kentucky must be at least $1 to achieve any health benefits," the coalition said in a news release. "Tobacco companies use coupons and other point-of-sale promotions to soften the impact of tax increases on the price of their products, so the tax increase has to be large enough to overcome those promotions."
"The current tax doesn't begin to cover the high cost of smoking in Kentucky," said KVH Executive Director Emily Beauregard. An extra dollar per pack will put a dent in those costs. More to the point of the coalition's work, it also will save lives and improve health."
"The current tax doesn't begin to cover the high cost of smoking in Kentucky," said KVH Executive Director Emily Beauregard. An extra dollar per pack will put a dent in those costs. More to the point of the coalition's work, it also will save lives and improve health."
Smoking's costs are measured not only in dollars, said Ben Chandler, chair of the coalition and CEO of the Foundation for a Healthy Kentucky, which staffs it. "Nearly 9,000 deaths every year in Kentucky are directly related to smoking, more than alcohol, AIDS, car crashes, illegal drugs, murders, and suicides combined," Chandler said. "If we don't start reducing smoking rates in Kentucky right now, 119,000 of today's youth will die early due to tobacco use."
The release said "5,900 Kentucky babies would be born healthier over a five-year period because their moms would quit smoking if the state enacted a $1 tax increase. The Campaign for Tobacco-Free Kids estimates that a total of 29,400 adults would quit smoking, and 23,200 kids would never start." The second page of the infographic appears below.
The release said "5,900 Kentucky babies would be born healthier over a five-year period because their moms would quit smoking if the state enacted a $1 tax increase. The Campaign for Tobacco-Free Kids estimates that a total of 29,400 adults would quit smoking, and 23,200 kids would never start." The second page of the infographic appears below.







