|
| Dr. Dan Goulson |
By Melissa PatrickKentucky Health News
As Covid-19 cases in Kentucky rose 22 percent last week and influenza killed 31 more Kentuckians, including three more children, physicians encouraged Kentuckians to follow tried and true public-health measures and to get their annual flu vaccine and updated Covid-19 booster shots.
The doctors from Lexington's three largest hospitals urged people to protect themselves and others during the holidays, with a special warning to protect the elderly, who are being affected differently from Covid-19 these days.
"It's not too late," said Dr. Dan Goulson, chief medical officer for CHI St. Joseph Health. "You can see some benefit from the vaccine within a few days. And so, if people are questioning whether they want to get the vaccine, they should get it and not convince themselves that it's too late."
 |
| Dr. Mark Spanier |
Dr. Mark Spanier, chief of emergency medicine at
Baptist Health Lexington, said about Covid, "We're seeing a lot more generalized weakness in the elderly . . . profound weakness leading to falls, leading to hip fractures, leading to just generalized stability, which can lead to other infections, pneumonia, urinary tract infections, and other more serious things for the elderly."
Spanier encouraged seniors who are getting progressively weaker to get tested for these diseases, even if they don't have respiratory symptoms. "If you get in that shape, make sure you seek medical care," he said.
Goulson said it's important to remember that flu, Covid-19 and respiratory syncytial virus (RSV), which is most dangerous to seniors and infants, are spread by droplets produced when we talk, cough, laugh and sing.
"That means that if you’re sick, the best thing to do to help keep other people from getting sick is to either mask or to isolate or both … and if you’re not sick and need to protect yourself, the best thing to do is to mask and to maintain social distancing,” Goulson said.
 |
| Dr. Gena Cooper |
Dr. Gena Cooper added frequent hand washing to that list, for both adults and children. "Those are all the things that still make the biggest difference, and are often the things you can individually control," said Cooper, emergency medical director at
Kentucky Children’s Hospital at the
University of Kentucky,
Goulson acknowledged that vaccines don't keep everyone from getting sick, and that sometimes creates skepticism, but said it's still important to get the shots because they keep people from getting sick enough to require hospitalization.
He pointed to two Centers for Disease Control and Prevention studies, released last week, that found the new bivalent Covid booster shots are more effective at reducing risk of hospitalization than boosters of the original version. The updated booster targets both the Omicron variants and the original virus strain to offer broader protections.
One of the studies showed a 45% lower risk of hospitalization among people who had gotten the updated booster, compared with people who received two to four doses of the original vaccine and received their last shot 11 or months earlier. The
other study showed a 73% reduction in hospitalization among people 65 and older who had gotten the latest, updated booster, compared to those who had gotten two to four doses of the original vaccine.
Studies have also found that the flu vaccine prevents severe illness for both adults and children, with a recent
study showing that it reduces children's risk of severe life-threatening flu by 75%.
Cooper, of the children's hospital, noted that while RSV rates are declining in Kentucky, the virus is still infecting Kentucky's children and most strongly affects those younger than 2.
She said she calls RSV "the mucus monster" because it creates so much mucus, which young children especially have trouble clearing from their respiratory system. She encouraged parents to use a bulb syringe after inserting a drop or two of nasal saline in each nasal cavity to help suction the mucus at home, especially before meals and at bedtime.
She added that cases of flu and RSV had "almost flip-flopped" at the children's hospital, which is good news because there is a vaccine to protect children against the flu.
The three physicians said their hospitals are almost full, but said that shouldn't deter a person from seeking medical care if they need it, recognizing that there may be increased wait times or the possibility of being cared for temporarily from the lobby or in a hallway.
Spanier encouraged Kentuckians to seek care for minor illnesses, such as cold symptoms, at their doctor's office and to seek care in an emergency room "if you have any doubt that you might have something more serious going on." He noted that emergency rooms are generally less busy in the morning.
He also encouraged Kentuckians to us a pulse oximeter at home to assess their oxygen level and to help determine if they need emergent care: "If you're getting down to 90 [percent] or below, you definitely need to be seen in an emergency department."
Flu deaths spike; six children die recently
The
state's latest flu report shows that flu activity in Kentucky remains high, but decreased 13% from the prior week's report.
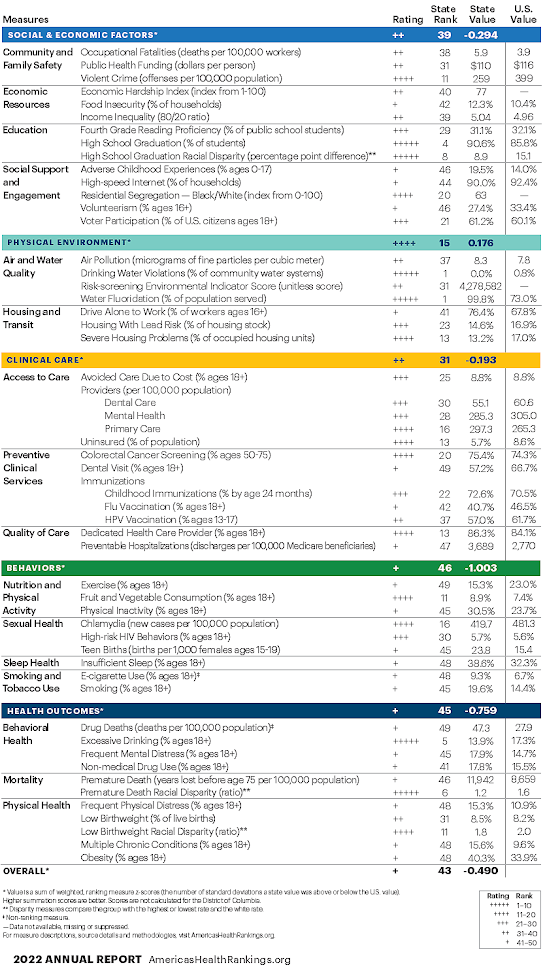
 |
| State Department for Public Health graph |
In the week ended Dec. 10, the state reported 6,240 confirmed cases of the flu, down from 7,192 the prior week. The total number of confirmed cases this flu season is 29,341. Most cases continue to be in people 20 and younger.
The report said the flu has killed at least 57 Kentuckians this season, three of them children. Of those deaths, 28 were reported in week ended Dec. 10 (27 adults and one child).
Since that report was compiled, the state has "reported six new, flu-related pediatric deaths, including three in the past week," said a press release from Gov. Andy Beshear late Monday afternoon. "This toll already meets the prior record for the highest number of pediatric influenza deaths ever reported in Kentucky in a single flu season. The prior record was established during the 2019-2020 flu season, when six children died of influenza."
As of Dec. 20, the state reports that six children total have died from the flu during the current 2022-2023 flu season.
The state
Department for Public Health said none of the children who have died this season had received a flu shot. “We are urging our families to get vaccinated as soon as possible to get protected from contracting the flu and Covid,” Beshear said.
Health Commissioner Steven Stack said, “This current flu season is on track to be the worst in Kentucky in at least 10 years. The flu vaccine is the single best way to protect you and your loved ones against the flu and reduces the risk of becoming dangerously ill or spreading disease. Unfortunately,
fewer than 40% of Kentucky children have received their flu shot this season. It is imperative that every Kentuckian take the essential steps to protect themselves, their loved ones and their communities.”
Several Kentucky counties saw 100 or more confirmed cases in the week ending Dec. 10, including Barren, 169; Boone, 413; Boyd, 109; Campbell, 220; Daviess, 171; Fayette, 276; Floyd, 184; Grant, 162, Jefferson, 1,170; Kenton, 573; Muhlenberg, 100; Perry, 116; Pike, 318; Warren, 122; and Whitley, 111.
Covid cases up 22%, but hospital numbers stable
In the week ended Dec. 19, the state
Department for Public Health reported 6,376 new coronavirus cases, an average of nearly 911 per day. That's 22% more than the week before, when the state was averaging 745 per day. Of last week's cases, 13% were in people 18 and younger.
The state attributed 45 more deaths from Covid-19, bringing the state's pandemic death toll to 17,625.
The share of Kentuckians testing positive for the virus in the last seven days was 9.85%, up more than a percentage point from the prior week's rate of 8.63%. The figures do not include at-home tests.
Covid-19 hospitalizations have been stable for two weeks in a row. Hospitals reported 370 patients with Covid-19 Monday morning, a decrease of 18 over the prior Monday; 42 were in intensive care, down three; and 20 were in need of mechanical ventilation, up one.
The weekly new-case incidence rate was 16.08 cases per 100,000 residents, up from 15.82 the week before. The top 10 counties are Calloway, 37.7 per 100,000; Crittenden, 37.3; Caldwell, 37; Monroe, 30.9; Leslie, 30.4; Carlisle, 30; Lyon, 29.6; Simpson, 29.2; Spencer, 27.3; and Powell, 26.6.
Kentucky's incidence rate 31st among the states, with a 21% increase in cases in the last two weeks.